We offer medical detox and multiple addiction treatment options in our
luxury treatment centres in Port Hope, Cobourg, and Ottawa.
What Is Opioid-Induced Wooden Chest Syndrome?
Wooden chest syndrome (WCS) represents one of fentanyl's most frightening effects. Your chest muscles lock tight. Breathing becomes impossible, even with assistance. This dangerous reaction stems from how synthetic opioids interact with your brain's receptors, creating a cascade of muscle rigidity that can prove fatal within minutes.

Thoracic and abdominal muscles bear the brunt of this condition, though your jaw, neck, and limbs can also freeze. Medical professionals first documented this phenomenon in 1953, but it's gained renewed urgency as Canada battles a devastating opioid overdose crisis.
Key Takeaways:
- How fentanyl attacks breathing through two separate pathways — one that naloxone can reverse, and one that it often can't
- The warning signs that appear within minutes — critical symptoms that demand immediate emergency response
- Why standard CPR fails when the chest muscles lock completely rigid
- The tolerance myth that kills experienced users — why decades of opioid use offers zero protection
- The hidden connection to Canada's contaminated drug supply — how people consume fentanyl without knowing it
- Why years of opioid experience offer zero protection — the tolerance paradox that makes everyone vulnerable
How Does Fentanyl Trigger Muscle Rigidity?
The biological explanation reveals why this complication proves so difficult to reverse. Fentanyl binds to μ-opioid receptors in your central nervous system. This triggers a dopaminergic pathway that leads directly to skeletal muscle rigidity. Your noradrenergic and cholinergic systems activate, reducing chest wall compliance and increasing muscle tension.

This happens through a non-opioid pathway, which separates chest wall rigidity from typical respiratory depression. That distinction becomes critical during treatment.
Fentanyl Crosses the Blood-Brain Barrier Quickly
Fentanyl's chemical structure makes it highly lipophilic. That scientific term means it dissolves easily in fat. Your brain contains substantial fatty tissue protecting it behind the blood-brain barrier. Fentanyl crosses this barrier faster than other opioids, delivering concentrated effects to your central nervous system within seconds.
Research suggests an active transporter may further increase fentanyl levels in your brain. These combined properties explain why fentanyl blockade produces more severe muscle rigidity than equivalent doses of morphine or heroin.
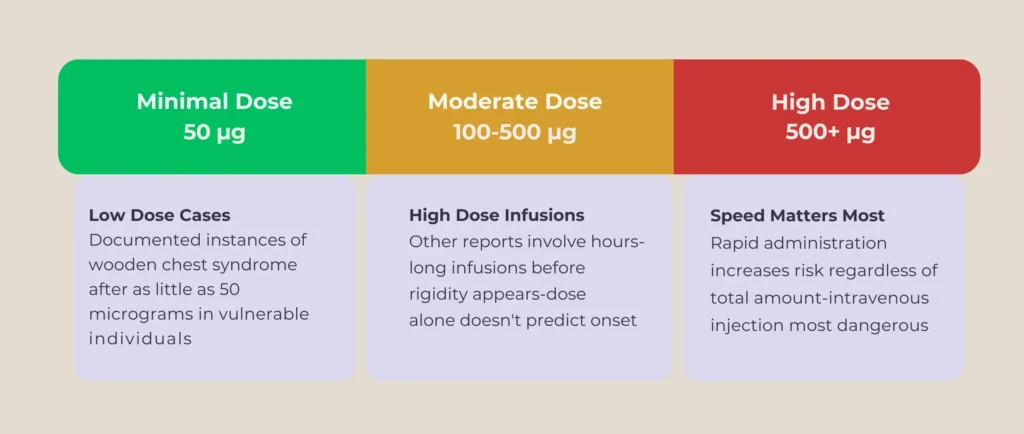
The Dose Controversy
Scientists debate whether dose determines severity. Some cases show rigidity developing after minimal fentanyl exposure, as little as 50 micrograms in documented instances. Other reports involve high-dose infusions continuing for hours before symptoms appear. Rapid administration seems to increase risk regardless of the total amount.
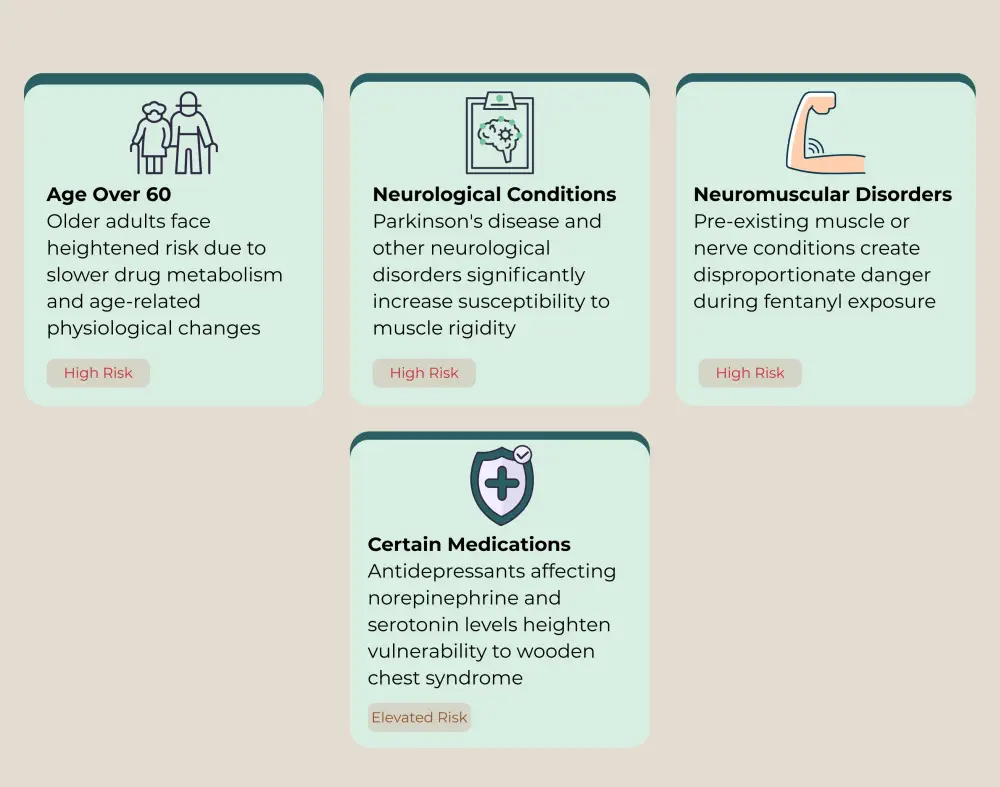
Individual Vulnerability Patterns
Your age, health conditions, and medications all influence susceptibility. Age over 60 years, underlying neurological conditions, Parkinson's disease, and certain antidepressant medications all heighten vulnerability. People with neuromuscular disorders face disproportionate danger.
What Are the Warning Signs of Wooden Chest Syndrome?
Immediate Physical Symptoms
Recognizing this emergency early can save lives. Wooden chest syndrome announces itself through episodic breath-holding spells. Your respiratory muscles contract and stay contracted. Your chest feels locked. Abdominal muscles turn rock-hard to the touch. Your jaw clamps shut.Observers notice your lips and face turning blue from oxygen deprivation. Cyanosis appears within seconds as your blood oxygen drops. Hypertension often accompanies these episodes. Your blood pressure spikes as your body struggles against the rigidity.

Ventilator Alarm Patterns
If you're on a ventilator, the machine starts alarming. Peak airway pressures climb dramatically, sometimes exceeding 60 cmH₂O, while normal values are around 20 cmH₂O.
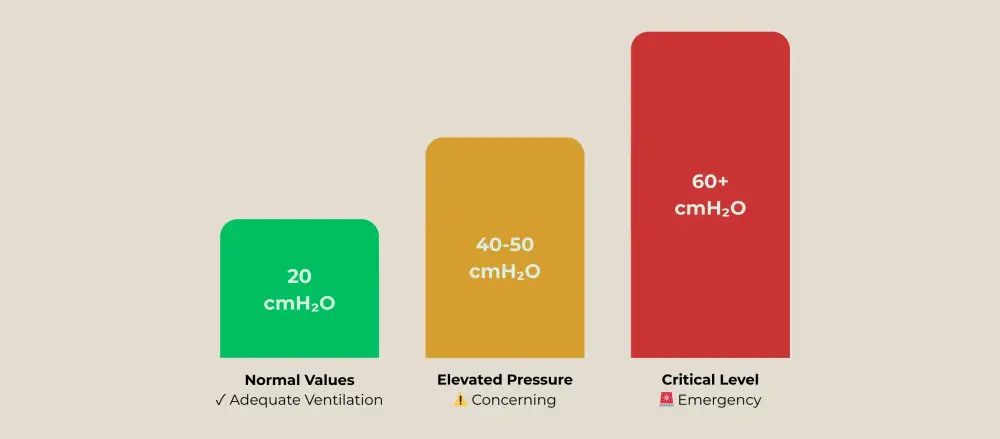
The ventilator works harder and harder but can't deliver adequate air. Bag-valve-mask ventilation meets tremendous resistance.
Critical Timing Windows
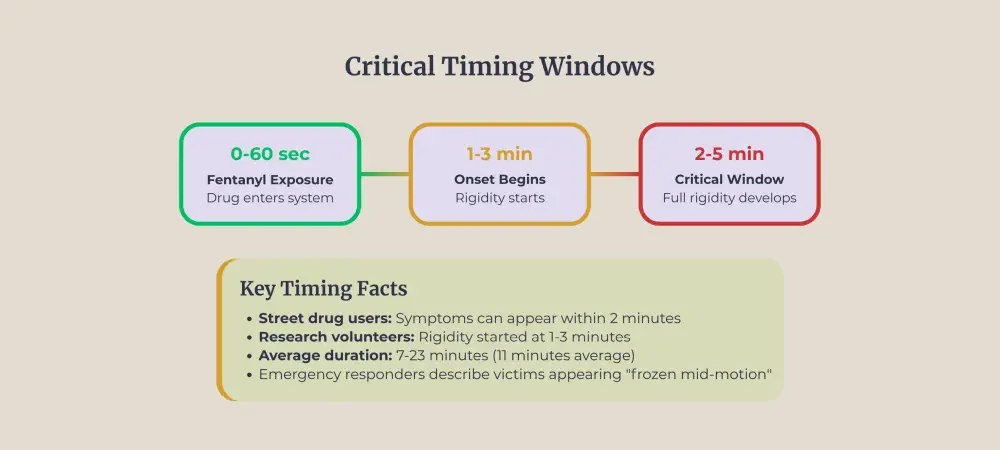
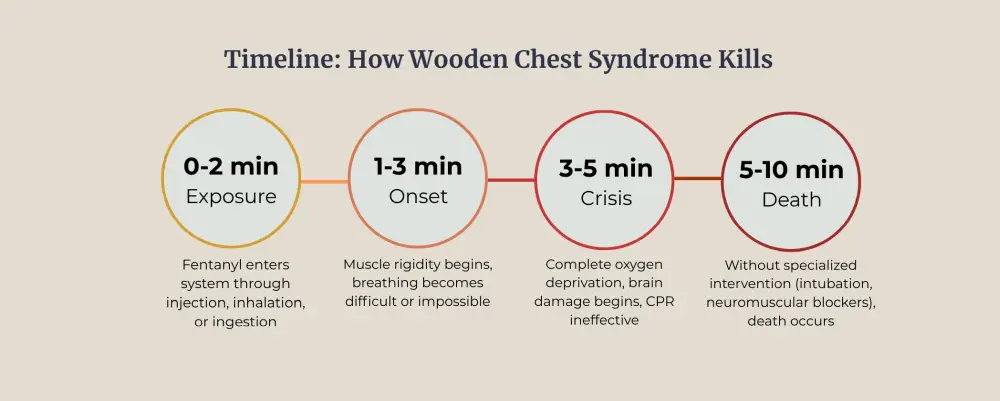
Timing provides crucial diagnostic clues. Chest wall rigidity strikes within minutes of fentanyl administration. Studies tracking healthy volunteers found rigidity starting approximately 1 to 3 minutes after injection. Duration averaged 11 minutes but ranged from 7 to 23 minutes in research subjects.
Street drug users experience an even faster onset. When someone smokes or injects illicit fentanyl, muscle rigidity can develop within two minutes. Emergency responders describe arriving at scenes where victims appear frozen mid-motion.
Distinctive Body Positioning
Your extremities may stiffen into unusual positions. Elbows flex rigidly. Fists clench. Neck muscles create a locked, forward posture.
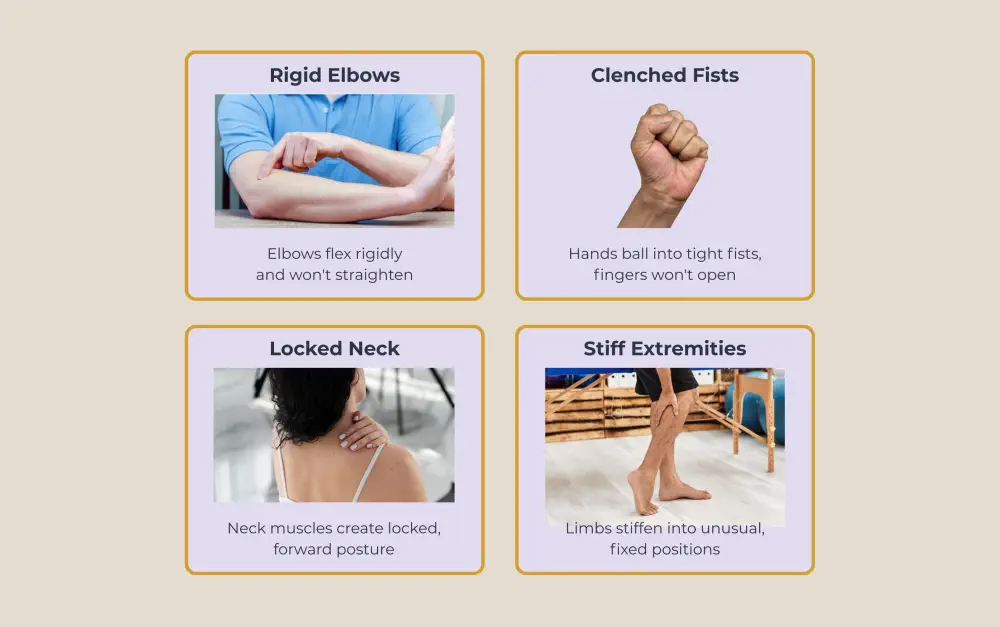
Some people exhibit what appears to be muscle spasms, but the contraction remains constant rather than rhythmic.
Airway Closure Complications
Laryngeal spasms occur in 50% to 100% of cases, depending on dosage and injection speed. Your vocal cords snap closed. Even skilled medical personnel struggle to insert breathing tubes when your throat muscles refuse to relax. These airway complications turn a serious emergency into an immediately life-threatening crisis.
Why Is WCS So Dangerous During an Opioid Overdose?
The symptoms described above turn lethal when combined with fentanyl's other effects. Fentanyl overdose victims often die before help arrives. WCS accelerates this timeline dramatically. Your brain requires constant oxygen. Muscle rigidity cuts off that supply within minutes.
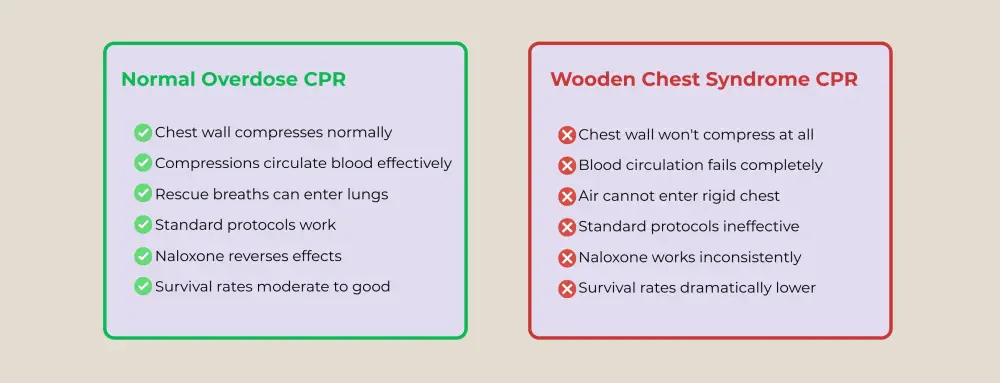
CPR Becomes Ineffective
Cardiopulmonary resuscitation becomes nearly impossible when chest muscles won't compress. First responders push down on a chest wall that won't give. Their compressions fail to circulate blood effectively. Emergency room survival rates for fentanyl overdoses run far lower than heroin overdoses for this exact reason.
Why Naloxone Fails
Naloxone works by blocking opioid receptors. It reverses respiratory depression caused through standard opioid pathways. But muscle rigidity operates through noradrenergic pathways that naloxone can't fully block. Some research suggests high naloxone doses might even worsen rigidity by upregulating noradrenergic release.
The fentanyl blockade of normal muscle function persists even after naloxone administration in many cases. Patients regain consciousness but remain unable to breathe independently. Medical teams must intubate and mechanically ventilate until the rigidity finally subsides.
Post-Mortem Evidence
Post-mortem examinations of sudden overdose deaths frequently reveal fentanyl present without its metabolite, norfentanyl. This finding indicates death occurred so rapidly that the body never began breaking down the drug. Research published in Clinical Toxicology suggests chest wall rigidity may explain some of these rapid fentanyl deaths, where traditional respiratory depression alone wouldn't kill quickly enough.
Canada's Contaminated Drug Supply
Canada's illicit opioid supply increasingly contains toxic synthetic opioids. As of 2022, important regional differences existed. British Columbia saw 84.7% of seized opioid samples containing fentanyl or analogues. Even in Atlantic Canada, with the lowest rates, 15.8% contamination was reported. Carfentanil—100 times more potent than fentanyl—appeared in nearly 20% of Alberta's opioid samples.
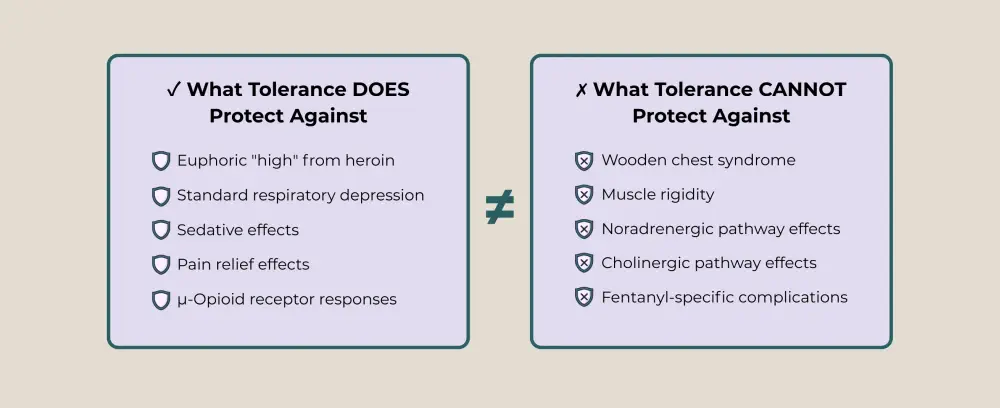
The Tolerance Paradox
Someone with decades of opioid addiction experience builds tolerance to heroin's euphoric effects and respiratory depression. However, this tolerance offers zero protection against wooden chest syndrome (WCS). The rigidity pathway operates independently via noradrenergic and cholinergic mechanisms rather than via standard μ-opioid receptor mechanisms. A person who safely used heroin for years can experience fatal muscle rigidity from their first fentanyl-contaminated dose.
What Is the Connection Between Wooden Chest Syndrome and Opioid Dependence?
Opioid addiction creates multiple pathways to wooden chest syndrome exposure. Medical patients receiving prescription fentanyl face risks during hospital procedures. People using illicit opioids encounter contaminated street drugs. Both groups need specialized understanding and support.
Prescription fentanyl addiction often begins with legitimate pain management. Doctors prescribe this powerful opioid for severe pain, post-surgical recovery, or chronic conditions. Within weeks of regular use, tolerance builds. Physical dependence follows. Some patients escalate dosing beyond medical recommendations, leading to increased muscle rigidity with continued use.
Drug dealers cut heroin or cocaine with fentanyl to increase potency cheaply. Someone purchasing what they believe is heroin may actually consume fentanyl. Even experienced users with established opioid dependence can't gauge dosing accurately when substances are mislabelled.
The link between muscle rigidity emergencies and opioid dependence underscores why substance use disorders demand specialized medical intervention. Recovery requires more than willpower—it demands medical care, psychological support, and community resources working in concert.

What Should You Do If You're Concerned About WCS?
Wooden chest syndrome represents one of fentanyl's most dangerous complications, creating rapid death through muscle rigidity that naloxone often can't reverse. Recognition of this condition helps families, first responders, and medical professionals recognize and respond to this emergency.
If you or someone you care about struggles with opioid addiction, professional treatment significantly improves survival odds and long-term recovery. The Canadian Centre for Addictions provides comprehensive care addressing both substance use disorders and the unique dangers of today's contaminated drug supply.
Contact the Canadian Centre for Addictions at 1-855-499-9446. Our experienced team can evaluate your situation and create a personalized plan addressing both immediate safety concerns and long-term recovery needs.
FAQ
Can wooden chest syndrome happen with other opioids?
Wooden chest syndrome occurs primarily with fentanyl and its analogues like sufentanil, remifentanil, and carfentanil. Traditional opioids like morphine and heroin rarely cause significant muscle rigidity. The high lipophilicity of fentanyl-class drugs allows rapid brain penetration, making them specifically dangerous for this complication.
What should bystanders do if they suspect wooden chest syndrome?
Call 911 immediately and state you suspect fentanyl exposure. Administer naloxone if available, but don't delay emergency services. Don't attempt CPR if the chest won't compress—wait for paramedics. Stay with the person and monitor breathing. If they regain consciousness but still can't breathe normally, they need immediate hospital care.
How do hospitals differentiate wooden chest syndrome from other respiratory emergencies?
Emergency physicians look for sudden onset within minutes of fentanyl exposure, a rigid abdomen and chest wall, extremely high ventilator pressures without airway obstruction, and failure to respond to naloxone. The combination of muscle rigidity, recent fentanyl exposure, and ineffective ventilation despite clear airways confirms the diagnosis.
Can wooden chest syndrome happen from fentanyl patches or pills?
Documented cases almost exclusively involve intravenous or inhaled fentanyl due to rapid central nervous system delivery. Properly used transdermal patches release medication slowly, making this complication extremely unlikely. However, people who chew, inject, or smoke extracted patch contents face identical risks. Counterfeit pills crushed and snorted or injected can trigger muscle rigidity.
What happens after surviving wooden chest syndrome?
Most survivors recover fully within 10-20 minutes with proper treatment. Patients remain hospitalized for 24-48 hours for monitoring. Prolonged oxygen deprivation can cause brain damage if intervention is delayed. This near-death experience often catalyzes entry into addiction treatment. Follow-up care should include addiction counselling and cognitive impairment screening.
Article sources
- Torralva, R., & Janowsky, A. (2019). "Noradrenergic Mechanisms in Fentanyl-Mediated Rapid Death Explain Failure of Naloxone in the Opioid Crisis." Journal of Pharmacology and Experimental Therapeutics, 371(2), 453-475. Available at: https://jpet.aspetjournals.org/content/371/2/453
- Baldwin, N., et al. (2022). "Regional variation in fentanyl contamination of the unregulated drug supply: Findings from a systematic review and meta-analysis." Drug and Alcohol Dependence, 233, 109366. Available at: https://www.sciencedirect.com/science/article/abs/pii/S0376871622000680
- Kinoshita, H., et al. (2020). "Postmortem toxicology of fentanyl and norfentanyl: Significance in forensic diagnosis of death." Forensic Science International, 316, 110475. Available at: https://www.sciencedirect.com/science/article/abs/pii/S0379073820303467
- Special Advisory Committee on the Epidemic of Opioid Overdoses. (2024). "Opioid- and Stimulant-related Harms in Canada." Public Health Agency of Canada. Available at: https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/
- Armenian, P., et al. (2018). "Fentanyl, fentanyl analogs and novel synthetic opioids: A comprehensive review." Neuropharmacology, 134, 121-132. Available at: https://www.sciencedirect.com/science/article/abs/pii/S0028390817303866
- Henderson, G.L. (1988). "Fentanyl-related deaths: demographics, circumstances, and toxicology of 112 cases." Journal of Forensic Sciences, 36(2), 422-433. Available at: https://pubmed.ncbi.nlm.nih.gov/1939747/
- Rzasa Lynn, R., & Galinkin, J.L. (2018). "Naloxone dosage for opioid reversal: current evidence and clinical implications." Therapeutic Advances in Drug Safety, 9(1), 63-88. Available at: https://journals.sagepub.com/doi/full/10.1177/2042098617744161
- British Columbia Coroners Service. (2024). "Illicit Drug Toxicity Deaths in BC: Findings Report." BC Government Publications. Available at: https://www2.gov.bc.ca/gov/content/life-events/death/coroners-service/statistical-reports
- Somerville, N.J., et al. (2017). "Characteristics of fentanyl overdose — Massachusetts, 2014–2016." MMWR Morbidity and Mortality Weekly Report, 66(14), 382-386. Available at: https://www.cdc.gov/mmwr/volumes/66/wr/mm6614a2.htm
- Strang, J., et al. (2019). "Opioid use disorder." Nature Reviews Disease Primers, 5(1), 1-28. Available at: https://www.nature.com/articles/s41572-019-0137-5






