We offer medical detox and multiple addiction treatment options in our
luxury treatment centres in Port Hope, Cobourg, and Ottawa.
How Mixing Adderall and Alcohol Affects Your Health
Prescription medications serve medical needs. Adderall helps millions manage ADHD symptoms effectively when taken as directed. Alcohol remains legal for adults across Canada. But combining these two substances creates serious health risks that many people don't realize until they face medical emergencies.

Students might mix Adderall and alcohol to study longer while still enjoying social events. Someone with a legitimate prescription might assume one drink poses no harm. These scenarios happen daily, yet the drug interaction between stimulants and depressants can trigger cardiovascular emergencies, severe alcohol intoxication, and long-term health consequences that extend far beyond a single night.
Key Takeaway:
- Why the "balancing out" myth is deadly — Discover how Adderall masks alcohol's warning signs instead of cancelling its effects, leaving you dangerously unaware as your blood alcohol climbs to poisoning levels.
- What happens to your heart under dual attack — See why previously healthy 20-somethings end up in cardiac ICU after mixing these substances, and how the combination creates stress your heart can't handle.
- How quickly things go from fine to emergency — Understand the critical time gap between feeling sober and requiring immediate medical intervention, and why friends often wait too long to call for help.
- Which behavioural changes signal serious danger — Recognize the personality shifts, decision-making failures, and memory blackouts that distinguish this combination from alcohol alone.
- When recreational use crosses into dependency — Identify the patterns that transform occasional mixing into polysubstance abuse requiring professional intervention.
What Happens When You Mix a Stimulant with a Depressant?
Adderall and alcohol work in opposite directions within your body. Adderall, containing amphetamine and dextroamphetamine, speeds up your central nervous system. Heart rate climbs. Blood pressure rises. Mental alertness sharpens. Alcohol does the reverse—slowing brain activity, reducing inhibitions, and impairing coordination.
The Dangerous Myth of Balance
Many people mistakenly believe these opposing forces balance each other out. They assume Adderall's energizing effects of Adderall will counteract alcohol's sedating qualities. This dangerous myth drives much of the mixing behaviour, particularly among college students trying to extend their drinking sessions without feeling tired.
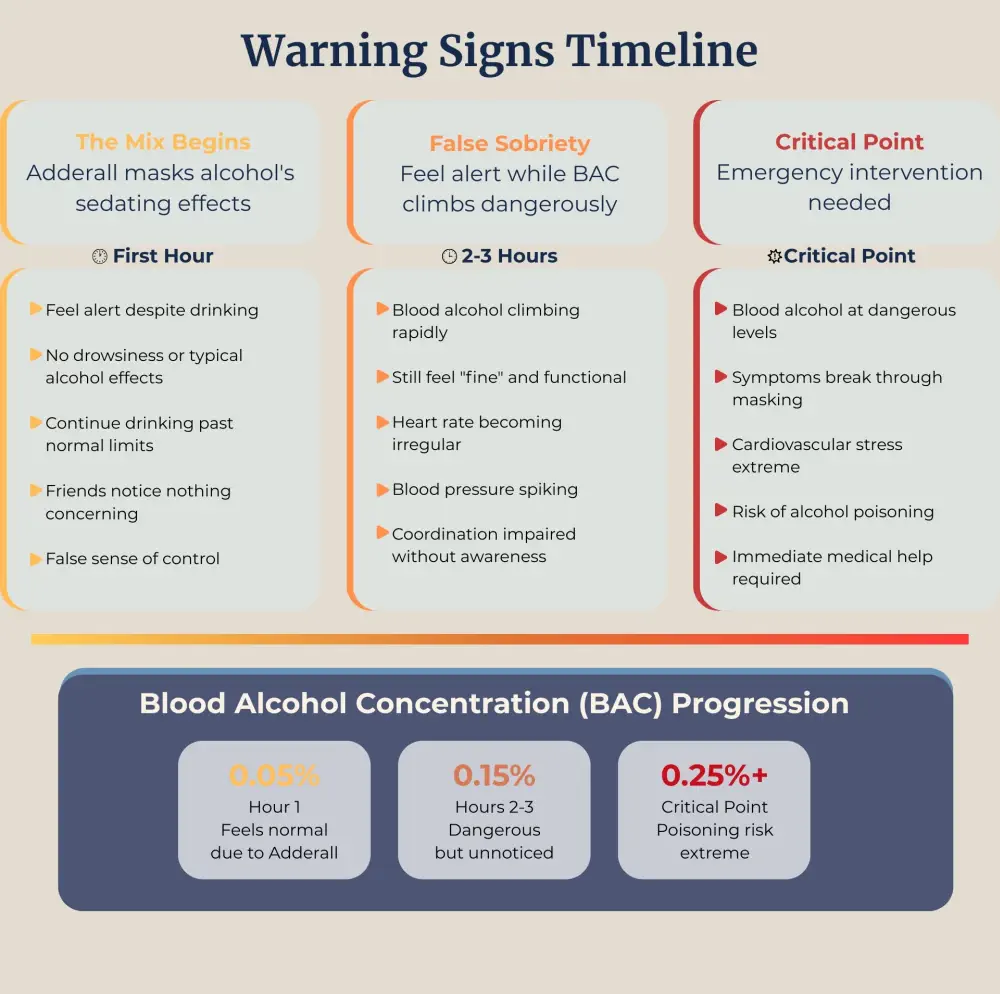
The reality works differently. Neither substance cancels the other. Adderall masks alcohol's warning signals. Your body normally sends clear messages when you've consumed too much alcohol: drowsiness, loss of coordination, and slurred speech. These symptoms act as natural brakes, typically prompting you to stop drinking before reaching dangerous levels.
How Masking Effects Create False Sobriety
Adderall strips away these protective warnings. You might feel alert and coordinated while your blood alcohol concentration climbs to hazardous levels. This drug interaction creates a false sense of sobriety that can lead directly to alcohol poisoning. Research shows people mixing these substances consistently drink more than they would with alcohol alone, often without recognizing their impairment.
Your liver processes both substances simultaneously, competing for the same metabolic pathways. Alcohol slows Adderall metabolism, keeping the stimulant in your system longer than expected. Higher Adderall levels amplify cardiovascular stress while you continue drinking beyond safe limits.
Why Does This Combination Threaten Your Heart?
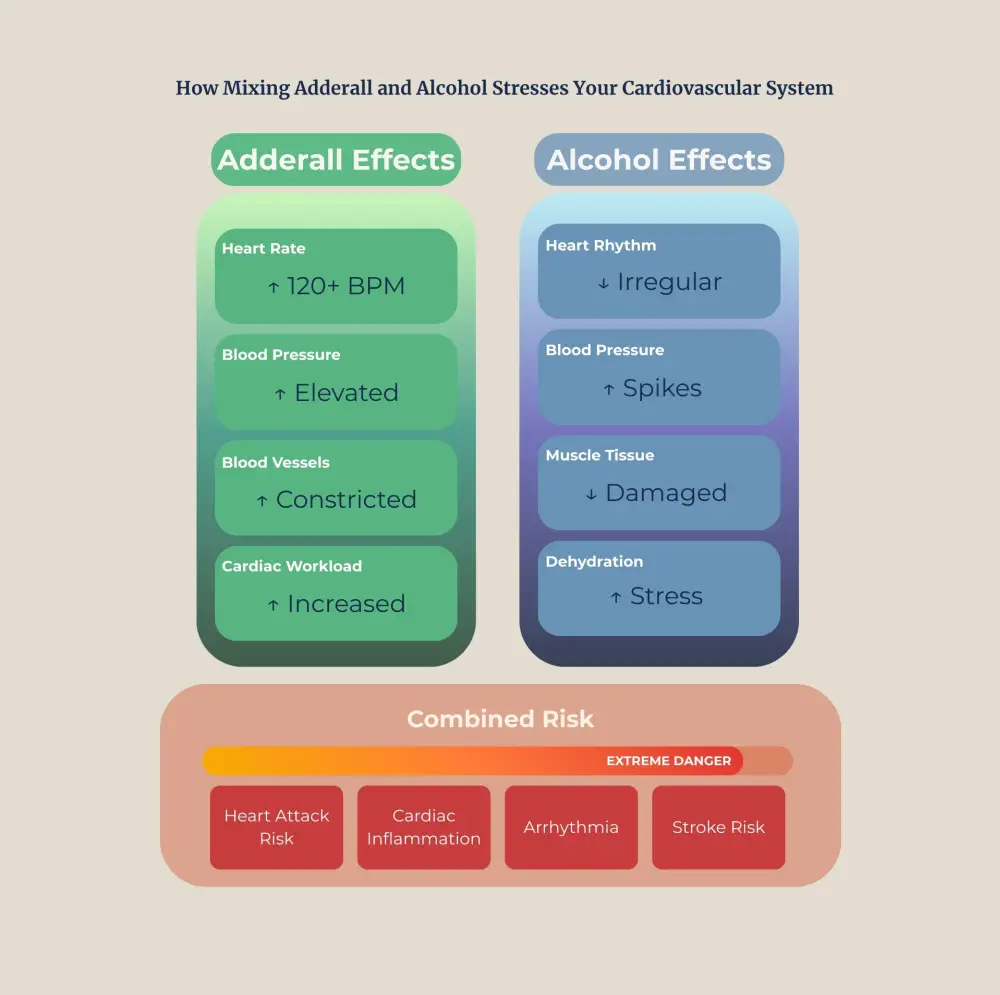
Cardiovascular complications represent the most severe immediate risk of mixing Adderall and alcohol. Both substances independently stress your cardiovascular system. Combining them multiplies these dangers exponentially.
Dual Cardiovascular Assault
Adderall triggers rapid heart rate increases and blood pressure spikes. These effects of Adderall occur even at prescribed doses but intensify with higher amounts. Your heart works harder, pumping faster, while blood vessels constrict from the stimulant's influence.
Alcohol adds its own cardiovascular burden. Despite initial blood vessel dilation that creates flushed skin, alcohol consumption raises blood pressure and disrupts normal heart rhythm patterns. Excessive intake damages heart muscle tissue over time.
Together, these substances force your heart into overdrive while simultaneously impairing its function. Blood pressure can reach dangerously high levels. Heart rate becomes erratic.
Studies have documented cases of previously healthy young adults experiencing heart attacks after combining Adderall with alcohol, some involving standard prescribed doses, not Adderall abuse. One published medical case described an adolescent who took their prescribed daily Adderall dose while drinking alcohol at a social event. Despite having no cardiovascular risk factors or history of heart problems, this person suffered an acute myocardial infarction requiring emergency treatment. The combination created such severe cardiovascular stress that normal heart tissue couldn't cope.
Progressive Heart Damage from Chronic Mixing
The risk extends beyond immediate heart attacks. Chronic mixing can lead to cardiomyopathy—progressive weakening of the heart muscle that occurs over months or years. Your heart struggles to pump blood effectively throughout your body. Early symptoms might include chest pain, irregular heartbeat, or unusual fatigue during normal activities.
How Does Alcohol Poisoning Risk Increase?
Alcohol intoxication becomes extremely dangerous when Adderall masks its symptoms. Your blood alcohol concentration can climb to potentially fatal levels while you feel relatively normal and continue drinking.
Missing the Warning Signs
Typical alcohol warning signs include severe drowsiness, confusion, vomiting, slowed breathing, and loss of consciousness. These symptoms prompt most people to stop drinking or seek help. Adderall's stimulant properties suppress many of these crucial alerts. You might maintain conversation, appear coordinated, and feel wide awake despite dangerously high blood alcohol levels.
Alcohol poisoning occurs when consumption overwhelms your body's ability to process it safely. Your breathing becomes dangerously slow or irregular. Body temperature drops. Severe dehydration sets in. Without prompt medical intervention, alcohol poisoning can cause permanent brain damage or death.
The Critical Time Gap
People mixing these substances often realize something's seriously wrong only when symptoms become severe enough to break through Adderall's stimulating effects. By that point, blood alcohol levels may require immediate emergency treatment. Friends might delay seeking help because the person seemed fine minutes earlier—creating critical time losses. Emergency responders recommend calling for help at the first signs of severe intoxication, even if the person seems relatively functional. Minutes matter when breathing becomes compromised or when someone loses consciousness.
College environments create particularly high-risk scenarios. Students might take Adderall to study, then switch to social drinking without considering how the medication still affects their system. Others intentionally combine both to "party longer" without recognizing the physiological dangers involved.
What Makes the Behavioural Risks Different from Alcohol Alone?
The drug interaction between Adderall and alcohol profoundly affects judgment, decision-making, and impulse control. Both substances independently impair these cognitive functions. Together, they create dangerous behavioural patterns that seem reasonable at the time but carry severe consequences.
Risky Decision-Making Amplified
Alcohol reduces inhibitions and impairs rational thinking. You might take risks you'd normally avoid—driving while impaired, engaging in unsafe sexual behaviour, or making financial decisions you'll regret. Adderall compounds these problems by adding false confidence and eliminating the fatigue that might otherwise slow your activities.
This combination frequently leads to aggressive behaviour and interpersonal conflicts. People report saying or doing things completely out of character during episodes of mixing. Relationships suffer. Legal troubles emerge. Some individuals engage in criminal behaviour they'd never consider while sober.
Psychological Reactions and Panic
The stimulant properties can also trigger severe anxiety or paranoia, particularly as Adderall's effects intensify due to slowed metabolism. Some people experience panic attacks requiring medical intervention. Others form disturbing thought patterns or hallucinations that persist beyond the immediate intoxication period.
Memory Blackouts While Appearing Functional
Memory problems create additional complications. You might have significant gaps in recollection from periods when you seemed functional to observers. These blackouts raise safety concerns and complicate efforts to piece together what occurred during intoxication.

How Does Non-Prescribed Use Amplify the Dangers?
Adderall abuse, taking medication without a prescription, using higher doses than prescribed, or consuming it through methods like snorting, dramatically escalates all these risks. Non-prescribed use often involves significantly higher doses than doctors would recommend, multiplying cardiovascular stress and other complications.
The Risks of Unmonitored Stimulant Use
People engaging in Adderall abuse frequently lack medical supervision. No healthcare provider monitors their heart function, blood pressure, or overall health response to the medication. Pre-existing conditions that would normally contraindicate Adderall use go undetected until emergencies occur.
Patterns of Polysubstance Use
The abuse patterns often coincide with heavy alcohol consumption. Students might obtain Adderall from friends specifically for extended drinking sessions. Others form polysubstance dependencies involving both stimulants and alcohol, creating addiction patterns requiring specialized treatment.
How Cross-Tolerance Accelerates Dependency
Tolerance builds with repeated Adderall abuse, driving users toward higher doses that increase cardiovascular risks. The body adapts to regular stimulation, requiring more medication to achieve the desired effects. Meanwhile, alcohol consumption may also escalate as the masking effects become familiar.
Dangerous Withdrawal from Both Substances
Withdrawal from both substances simultaneously creates severe physical and psychological challenges. Stopping Adderall after prolonged abuse triggers extreme fatigue, depression, and intense cravings. Alcohol withdrawal can cause life-threatening seizures and delirium tremens requiring medical management. Attempting unsupervised withdrawal from both substances simultaneously poses serious health risks.
What Warning Signs Indicate You Need Treatment?
Warning signs demanding immediate medical attention include chest pain, severe difficulty breathing, irregular heartbeat, confusion, loss of consciousness, or inability to wake someone who's been drinking. Don't wait to see if symptoms improve—cardiovascular emergencies and alcohol poisoning require urgent intervention.
Beyond acute emergencies, several patterns indicate you need professional support for substance use concerns. If you regularly combine Adderall and alcohol despite knowing the risks, struggle to control either substance independently, or notice your use affecting relationships, work, or health, these signals indicate problems requiring expert help.
Professional addiction treatment typically includes medically supervised detoxification, individual and group therapy, and comprehensive aftercare planning. Treatment programs addressing polysubstance dependencies provide the best outcomes when they treat both stimulant and alcohol issues together rather than separately.
FAQ
Can I drink alcohol if I take Adderall as prescribed?
No, you should avoid alcohol entirely during Adderall treatment, even with a legitimate prescription. The cardiovascular risks and potential for alcohol poisoning exist no matter how you obtained Adderall. Consult your prescribing physician about your specific situation and timing considerations.
How long should I wait after taking Adderall before drinking?
Adderall remains in your system for 9-14 hours, with complete elimination taking up to three days, depending on dosage and formulation. Extended-release versions last longer. Your doctor can provide personalized guidance based on your specific prescription, but avoiding alcohol entirely during treatment represents the safest approach.
What are the signs someone has mixed Adderall and alcohol dangerously?
Watch for chest pain, severe headache, extremely rapid heartbeat, difficulty breathing, confusion beyond typical intoxication, seizures, or loss of consciousness, even if someone appears functional. Excessive drinking while on Adderall creates poisoning risks. Seek medical help immediately if you notice concerning symptoms.
Does everyone who mixes these substances experience problems?
Not everyone faces immediate emergencies, but every instance carries serious risks. Some people experience complications the first time; others encounter problems after repeated mixing. Pre-existing heart conditions, higher doses, and frequent use increase dangers, but even healthy individuals can suffer heart attacks or poisoning.
Can treatment help if I've encountered problems with both substances?
Recovery is absolutely achievable with proper support. Treatment programs addressing polysubstance dependencies provide complete care for both stimulant and alcohol issues simultaneously. Medical supervision, therapy, and ongoing support help thousands of Canadians build healthy lives free from substance dependence each year.
Article sources
- Luderer, M., et al. (2021). "Attention-deficit/hyperactivity disorder and alcohol use disorder: Epidemiology, clinical presentation, and the role of pharmacotherapy." Neuroscience & Biobehavioral Reviews, 131, 726-741. Available at: https://pubmed.ncbi.nlm.nih.gov/34425162/
- Weyandt, L.L., et al. (2016). "Nonmedical prescription stimulant use among university students: relationships with psychological distress, personality, and attachment." Journal of American College Health, 64(7), 493-502. Available at: https://pubmed.ncbi.nlm.nih.gov/27149662/
- Barrett, S.P., et al. (2005). "The effects of alcohol intoxication on stimulus expectancy in amphetamine users." Addiction, 100(2), 182-190. Available at: https://pubmed.ncbi.nlm.nih.gov/15679748/
- Varga, M.D. (2012). "Adderall abuse on college campuses: a comprehensive literature review." Journal of Evidence-Based Social Work, 9(3), 293-313. Available at: https://pubmed.ncbi.nlm.nih.gov/22694138/
- Lakhan, S.E., & Kirchgessner, A. (2012). "Prescription stimulants in individuals with and without attention deficit hyperactivity disorder: misuse, cognitive impact, and adverse effects." Brain and Behavior, 2(5), 661-677. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC3489818/
- Benson, K., et al. (2015). "Misuse of stimulant medication among college students: a comprehensive review and meta-analysis." Clinical Child and Family Psychology Review, 18(1), 50-76. Available at: https://pubmed.ncbi.nlm.nih.gov/25575768/
- Westover, A.N., & Nakonezny, P.A. (2010). "Aortic dissection in young adults who abuse amphetamines." American Heart Journal, 160(2), 315-321. Available at: https://pubmed.ncbi.nlm.nih.gov/20691837/
- Kaye, S., et al. (2009). "Methamphetamine and cardiovascular pathology: a review of the evidence." Addiction, 102(8), 1204-1211. Available at: https://pubmed.ncbi.nlm.nih.gov/17565560/
- Mariani, J.J., & Levin, F.R. (2012). "Psychostimulant treatment of cocaine dependence." Psychiatric Clinics of North America, 35(2), 425-439. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC3370242/






