We offer medical detox and multiple addiction treatment options in our
luxury treatment centres in Port Hope, Cobourg, and Ottawa.
Compulsive vs Impulsive Behaviour in Addiction
Both patterns can spiral into drug addiction, though they travel different routes. The difference between compulsive and impulsive behaviours shapes how substance use problems develop and persist. One chases thrills. The other flees discomfort. Both can destroy lives.
Key Takeaways:
- Why does impulsive behaviour happen when your brain's "pause button" fails, preventing you from stopping before acting on dangerous urges
- How compulsive behaviour traps you in anxiety-driven loops where breaking established patterns feels genuinely impossible.
- Why most addiction to substances begins with impulsive experimentation but inevitably transforms into compulsive maintenance as your brain chemistry changes.
- Why treatment approaches targeting your specific brain pattern succeed while generic programs often fail completely.
- The predictable shift from "wanting" to "needing" in addiction—learn exactly when you can interrupt this progression.

What Is Impulsive Behaviour?
Impulsive behaviour means acting without thinking. Immediate rewards pull you forward. Consequences? They register later—sometimes much later.
Buying lottery tickets on a whim happens this way. So does texting while driving. Trying cocaine at a party because everyone else is. Snap decisions occur when your brain's reward system drowns out caution.
Neuroscience reveals something striking about impulsivity. The prefrontal cortex (your brain's decision-making center)
Shows reduced activity in highly impulsive people. Driving with faulty brakes provides an apt comparison. The car moves forward, while stopping becomes dangerously difficult.
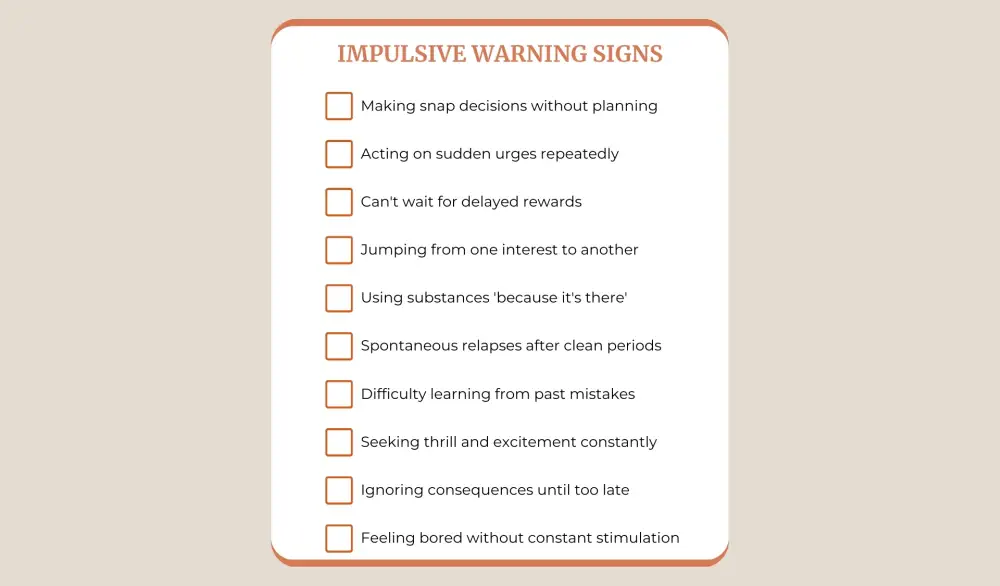
Common patterns include:
- Spur-of-the-moment decisions followed by regret
- Inability to wait for delayed gratification
- Acting on feelings without pause
- Jumping between interests rapidly
- Difficulty learning from past mistakes
This creates ideal conditions for experimenting with substances. That first drink feels spontaneous, not calculated. Deciding to try prescription pills happens in seconds rather than through careful consideration. Early drug addiction frequently begins with seemingly minor choices.
Research from addiction neuroscience demonstrates that impulsivity predicts escalation from casual use to problematic patterns. Your brain chemistry makes you vulnerable to the first step into substance use disorders.
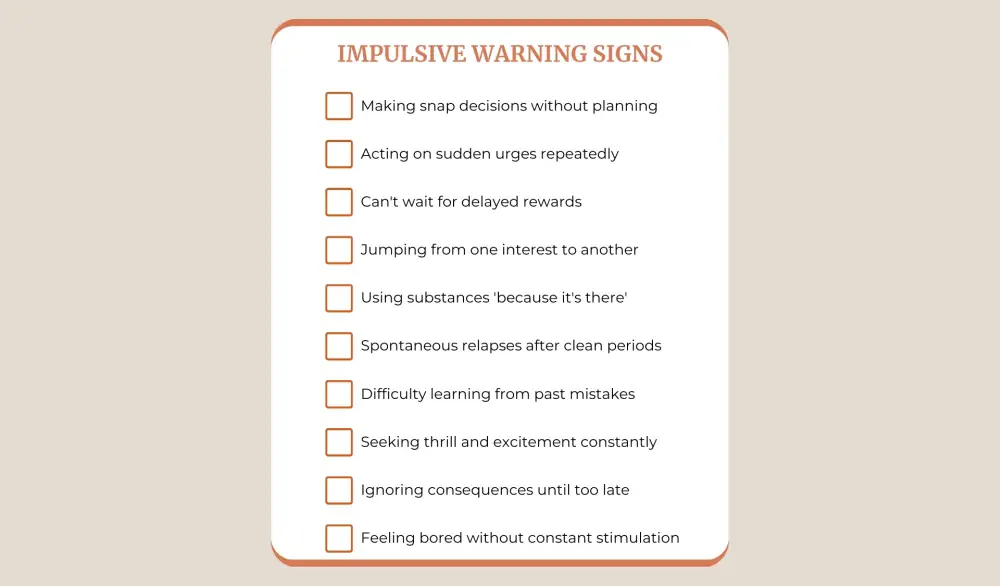
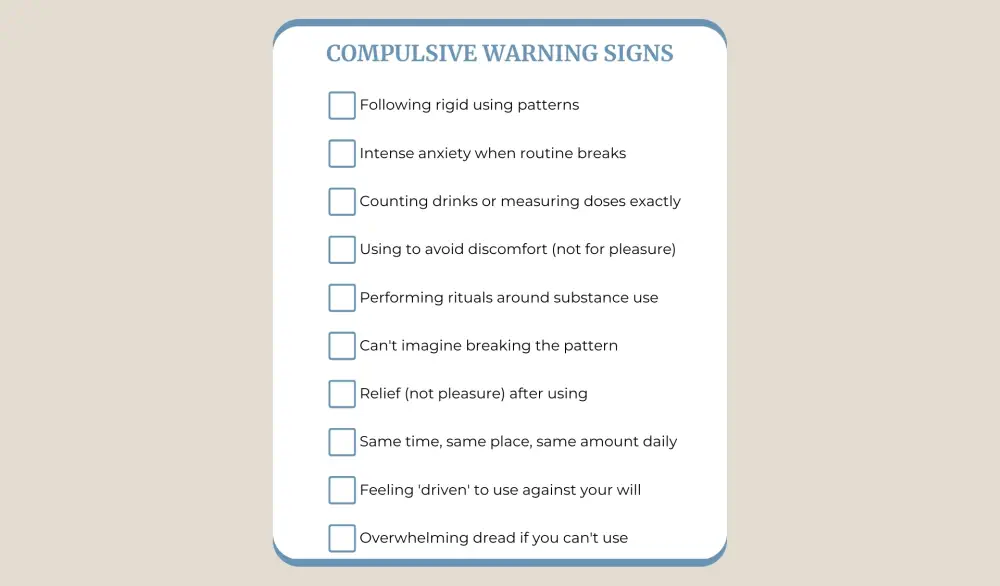
Identifying three or more signs from either column indicates a pattern emerging that typically requires professional intervention. Five or more suggests an established pattern. Seven or more often signals severe dependency requiring immediate attention.
What Defines Compulsive Behaviour?
Compulsive behaviour operates through entirely different machinery. You don't seek pleasure—you flee discomfort.
Crushing anxiety emerges unless specific rituals are performed. Washing hands seventeen times. Arranging items in exact patterns. Drinking precisely three beers nightly because breaking the pattern feels unbearable.
How compulsive and impulsive motivations differ runs deep. Compulsions reduce negative feelings. Impulses chase positive ones. One avoids pain while the other pursues pleasure.
The Brain's Role in Compulsivity
Brain imaging studies reveal something unexpected. While acting impulsively involves underactive prefrontal regions, these same areas show hyperactivity in compulsive patterns. Your brain works overtime managing perceived threats through repetitive actions.
Key characteristics include:
- Repetitive actions following rigid patterns
- Strong urges that feel impossible to resist
- Temporary anxiety relief after completing the behaviour
- Rituals serving no logical purpose
- Increasing time spent on these activities
When this intersects with substances, the pattern becomes self-perpetuating. Drinking calms anxiety. The drinking creates more anxiety. So you drink again. The cycle tightens like a noose.
Unlike the spontaneity of impulsive actions, compulsions feel driven by necessity. You're not choosing to use—you're compelled to. The substance becomes a tool for managing overwhelming internal distress.
Can You Predict When Casual Use Becomes Compulsive?
Addiction doesn't spring fully formed. It evolves.
Most drug dependencies begin with impulsive experimentation. Trying something new without fully considering risks. That initial use is driven by pleasure, curiosity, or social connection. Your prefrontal cortex fails to engage enough to slam the brakes.
How Addiction Changes the Brain
Addiction fundamentally changes brains. A large-scale study published in Frontiers in Psychiatry examined over 9,500 people with various behavioural addictions. The findings proved striking: in non-problematic users, impulsive and compulsive patterns appeared equally. But in severe addiction? Compulsivity dominated overwhelmingly.
The balance shifts as dependence deepens. Early addiction revolves around chasing that initial high—pure impulsivity. Using happens because it feels good, not because it's necessary. Decision-making occurs rapidly, driven by reward anticipation.
The Shift from Pleasure to Necessity
Then neurochemistry rewires itself. Dopamine pathways that once screamed "pleasure!" now whisper "survival." Substance use transitions from wanting to needing.
Later-stage drug addiction looks profoundly different. You're not using for pleasure anymore—avoiding withdrawal, anxiety, and psychological pain becomes the goal. The behaviour grows ritualistic, rigid. Breaking the pattern feels intolerable.
Research on opioid dependence demonstrates this clearly. Active users show heightened impulsive tendencies. Those in long-term recovery? Their brains reveal increased compulsive patterns persisting even after substance use stops. The impulsive drive may fade while compulsive patterns dig deeper roots.
This progression clarifies why treating established addiction requires addressing both dimensions. The impulsive triggers that started the pattern still exist. Meanwhile, compulsive maintenance mechanisms have grown equally powerful, sometimes more so.
Which Behaviours Lead More to Addiction?
Both pathways lead to drug addiction, but they predict different outcomes.
Impulsive behaviour acts as the gateway. Studies consistently show that high impulsivity precedes substance use initiation. Struggling to control impulses makes you statistically more likely to experiment with drugs initially. Your brain makes that first "yes" easier to say.
Compulsive behaviour predicts severity. Research proves that as addiction worsens, compulsivity dominates the clinical picture. People with the most severe substance use disorders display the strongest compulsive patterns. Their addiction evolved from casual to chronic, recreational to ritualistic.
The difference between compulsive and impulsive traits appears in relapse patterns. Impulsive individuals might suddenly use after months of being clean—a spontaneous decision they didn't plan. Those with compulsive tendencies return to rigid patterns, driven by overwhelming urges experienced as involuntary.
Genetic and Environmental Factors
Genetic research adds complexity. Certain variations in dopamine receptors increase the risk. Compulsive traits often develop through environmental factors—trauma, chronic stress, and untreated anxiety. Your starting point differs, yet both roads lead toward dependence.
Asking which is "worse" misses the point. Impulsive behaviour gets you started, while compulsive behaviour keeps you stuck. Early intervention works best for impulsive patterns. Intensive, long-term support becomes necessary once compulsivity establishes itself.
For families considering prevention, watch for both patterns. High impulsivity during adolescence warrants attention before experimentation begins. Rigid, anxiety-driven behaviours signal vulnerability even without current substance use.

Can Impulsive and Compulsive Patterns Be Reversed?
Effective addiction treatment must address both behavioural patterns, not merely the substance itself. If impulsive or compulsive behaviour is part of a disorder, management should be followed by a psychiatrist.
For those exhibiting impulsive traits, cognitive-behavioural therapy teaches critical pause-and-plan skills. You learn to recognize trigger moments—those split seconds before impulsive action. Techniques include:
- Delay strategies (waiting 10 minutes before acting on urges)
- Cost-benefit analysis training
- Mindfulness to increase awareness of impulses
- Medication to help regulate dopamine systems
Managing compulsive patterns requires different approaches. Treatment focuses on reducing the anxiety driving repetitive behaviours. Exposure therapy helps people tolerate discomfort without performing compulsive actions. Gradually, the overwhelming need to use lessens.
Recovery goes beyond willpower alone. It involves rewiring the brain mechanisms that make control so difficult. Whether impulsivity started your journey or compulsivity maintains it, professional help provides the tools for lasting change.
FAQ
What is the main difference between compulsive and impulsive behaviour in addiction?
Impulsive behaviour involves acting quickly without considering consequences, driven by reward-seeking. Compulsive behaviour means repeating actions to relieve anxiety or discomfort, even when they cause harm. Impulsivity chases pleasure while compulsivity flees pain.
Can someone have both impulsive and compulsive behaviours in addiction?
Yes, this combination appears extremely common in drug addiction. Most people start with impulsive patterns but develop compulsive ones as dependence deepens. The two often coexist, especially in moderate to severe substance use disorders.
Which behaviour pattern is harder to treat in addiction recovery?
Compulsive patterns typically prove more challenging because they're deeply rooted in anxiety management and negative reinforcement. While impulsive patterns can shift relatively quickly with skill-building, compulsive tendencies require extensive work addressing underlying emotional regulation and often persist even after substance use stops.
How can I tell if my substance use is driven by impulsivity or compulsivity?
Ask yourself: Do I use spontaneously without planning? Or do I feel overwhelming anxiety when I don't follow specific usage patterns? If use feels like a sudden decision, impulsivity likely drives it. When breaking your routine creates intense discomfort, compulsivity powers the behaviour.
How long does treatment typically take for impulsive versus compulsive addiction patterns?
Treatment duration varies significantly between patterns. Impulsive behaviour patterns often respond to short-term interventions (3-6 months) focused on skill-building and impulse-control strategies. Compulsive patterns typically require longer treatment (6-12 months or more) because they involve deeply rooted anxiety management systems.
Article sources
- Broos, N., et al. (2012). "The relationship between impulsive choice and impulsive action: a cross-species translational study." PLOS ONE, 7(5). Available at: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0036781
- Fineberg, N.A., et al. (2014). "Probing compulsive and impulsive behaviours, from animal models to endophenotypes: a narrative review." Neuropsychopharmacology, 39(7), 1707-1726. Available at: https://www.nature.com/articles/npp20148
- Verdejo-García, A., et al. (2008). "Impulsivity as a vulnerability marker for substance-use disorders: review of findings from high-risk research, problem gamblers and genetic association studies." Neuroscience & Biobehavioral Reviews, 32(4), 777-810. Available at: https://pubmed.ncbi.nlm.nih.gov/18295884/
- Koob, G.F., & Volkow, N.D. (2016). "Neurobiology of addiction: a neurocircuitry analysis." The Lancet Psychiatry, 3(8), 760-773. Available at: https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(16)00104-8/fulltext
- Albertella, L., et al. (2020). "Compulsivity is measurable across distinct psychiatric symptom domains and is associated with familial risk and reward-related attentional capture." CNS Spectrums, 25(4), 519-526. Available at: https://www.cambridge.org/core/journals/cns-spectrums/article/compulsivity-is-measurable-across-distinct-psychiatric-symptom-domains-and-is-associated-with-familial-risk-and-rewardrelated-attentional-capture/
- Everitt, B.J., & Robbins, T.W. (2016). "Drug addiction: updating actions to habits to compulsions ten years on." Annual Review of Psychology, 67, 23-50. Available at: https://www.annualreviews.org/doi/10.1146/annurev-psych-122414-033457






