We offer medical detox and multiple addiction treatment options in our
luxury treatment centres in Port Hope, Cobourg, and Ottawa.
What Are the Models of Addiction?
Addiction affects millions of people worldwide, yet experts have developed several competing frameworks to explain how and why it develops. These theoretical perspectives, known as models of addiction, each offer distinct explanations for the causes and patterns behind addictive behaviours. Patients, families, and healthcare professionals need these frameworks to choose effective paths to addiction recovery. Each model shapes treatment approaches differently, from medication-assisted programmes to therapy and peer support groups.
Key Takeaway:
- Why the moral model creates stigma — and how genetic research proves that 40-60% of addiction risk is inherited, not a character flaw
- When addiction became a legitimate medical condition — the year that opened doors to insurance coverage and professional treatment for millions
- What drives people to self-medicate — the connection between childhood trauma, mental health conditions, and substance dependence
- Which everyday situations program addictive responses — the conditioning patterns that happen without conscious awareness
- Which framework professionals actually use today — and why it addresses failures of earlier single-cause theories
What Is the Moral Model of Addiction?
The moral model of addiction frames substance dependence as a character flaw or failure of personal responsibility. According to this historical perspective, people who struggle with addiction lack self-discipline and make poor choices due to weak willpower.
This approach dominated Western thinking for centuries. Religious and cultural institutions viewed substance use as sinful behaviour requiring moral reformation. The model emphasizes personal agency—the idea that individuals freely choose to use substances and can simply choose to stop.

Some faith-based recovery programmes still incorporate elements of this framework today. They focus on spiritual change and personal accountability over medical intervention.
Why This Model Falls Short
Research has thoroughly discredited the moral model as a complete explanation. Genetic studies show that 40-60% of addiction risk stems from inherited traits. Brain imaging reveals measurable neurological changes in people with substance use disorders.
The moral model creates harmful stigma. When society views addiction as a character defect, people feel shame instead of seeking professional help. This perspective ignores biological vulnerabilities, trauma histories, and environmental influences that contribute to addictive behaviours.
Treatment based solely on willpower fails because it doesn't address the biological and psychological drivers of compulsive substance use.
What Are the Disease Models of Addiction?
Disease models of addiction treat substance dependence as a chronic medical condition with neurological and genetic foundations. The American Medical Association first recognized alcoholism as a disease in 1956, fundamentally changing how healthcare systems approach addiction.
This framework views addiction through the same lens as diabetes or heart disease—a long-term condition requiring ongoing medical management. People with substance use disorders experience measurable changes in brain chemistry, particularly in dopamine pathways that regulate reward and motivation.
The disease model highlights genetic predisposition. Twin studies and family research demonstrate that addiction runs in families, independent of environmental factors. When someone with a genetic vulnerability uses substances, their brain responds differently from someone without this predisposition.
How Disease Models Shape Treatment
Medical interventions form the cornerstone of disease-based treatment. Medications like methadone, buprenorphine, and naltrexone target specific brain receptors to reduce cravings and withdrawal symptoms. Patients receive ongoing monitoring similar to other chronic conditions.
This approach dramatically reduced stigma by reframing addiction as a health issue rather than a moral failure. Insurance companies began covering treatment. Healthcare providers developed evidence-based protocols.
Behavioural therapies complement pharmaceutical interventions. Cognitive-behavioural therapy helps patients develop coping strategies as medications stabilize brain chemistry.
How Can the Disease Model Oversimplify Addiction
Critics argue that the disease model can oversimplify addiction. Focusing exclusively on biology may neglect psychological trauma, social circumstances, and learned behaviours that maintain substance use. Some worry the framework promotes helplessness—if addiction is purely a brain disease, can people truly recover?
The model works best when integrated with other perspectives instead of being applied in isolation.

How Do Psychological Models Explain Addiction?
Psychological models connect addictive behaviours to mental health conditions, unresolved trauma, and emotional regulation difficulties. These frameworks explore how people turn to substances to manage psychological distress.
Self-medication theory represents a core concept. People with depression, anxiety, or post-traumatic stress disorder often discover that substances temporarily relieve symptoms. What begins as coping becomes compulsive use.
Research on adverse childhood experiences (ACEs) reveals strong correlations between early trauma and later addiction. Neglect, abuse, household dysfunction, and violence increase vulnerability to substance dependence. The psychological wounds from these experiences drive people toward external solutions for internal pain.
Personality traits also play a role. Impulsivity, sensation-seeking, and difficulty managing emotions all increase addiction risk.
What Psychological Interventions Treat Addiction
Therapy addresses root causes, not merely symptoms. Cognitive-behavioural therapy helps people identify triggers, challenge distorted thinking, and develop healthier coping mechanisms. Trauma-focused interventions process painful experiences that fuel substance use.
Dual diagnosis treatment handles co-occurring mental health conditions alongside addiction. Treating only the substance use but ignoring depression or anxiety leads to relapse.
The psychological model empowers people to understand their behaviour patterns and develop genuine emotional regulation skills.
What Is the Environmental Model of Addiction?
Social and environmental models emphasize that addictive behaviours are learned through observation, peer influence, and cultural context. People develop substance use patterns based on what they observe and experience in their social environments.
Albert Bandura's social learning theory explains how people learn by watching others. Children who grow up in households where substance use is normalized are more likely to develop similar patterns. They absorb behaviours, attitudes, and coping strategies from their family environment.
Classical conditioning explains why environmental cues trigger intense cravings. Someone who always used cocaine at parties may experience overwhelming urges when entering similar social situations. The brain associates specific places, people, and circumstances with substance use.
Operant conditioning involves reinforcement. The pleasurable effects of substances provide positive reinforcement. Using substances to avoid withdrawal symptoms creates negative reinforcement. Both processes strengthen addictive patterns.
Social Approaches to Recovery
Peer support groups like Alcoholics Anonymous and Narcotics Anonymous apply social learning principles. Members observe others successfully maintaining sobriety and model these behaviours.
Family therapy addresses dysfunctional dynamics that enable or encourage substance use. When family members stop "rescuing" someone from the consequences of their addiction, natural consequences provide powerful motivation for change.
Environmental modifications reduce exposure to triggers. This might mean changing social circles, avoiding certain locations, or restructuring daily routines.
Cue exposure therapy gradually reduces the power of environmental triggers by repeatedly exposing people to cues without allowing substance use.

What Is the Biopsychosocial Approach to Addiction?
The biopsychosocial model integrates biological, psychological, and social dimensions into a unified framework for explaining models of addiction. Developed in the 1970s by psychiatrist George Engel, this approach recognizes that addiction emerges when multiple influences interact across different domains.
The biological component includes genetics, brain chemistry alterations, and neurological changes. Some people have naturally lower dopamine levels, making substances feel more rewarding. Others have genetic variations affecting how they metabolize drugs or alcohol.
Psychological influences encompass mental health conditions, trauma histories, personality traits, and learned coping patterns. Depression, anxiety, and PTSD frequently co-occur with substance use disorders.
Social dimensions cover family dynamics, peer relationships, socioeconomic status, cultural norms, and access to substances. Poverty, unemployment, and social isolation all increase addiction risk.
The Significance of Integration
No single influence determines whether someone develops addiction. The biopsychosocial model acknowledges that each person's pathway is unique. One individual might have strong genetic loading but protective social support. Another might have minimal biological vulnerability but severe trauma and peer pressure.
This unified view allows for truly personalized treatment. Clinicians assess all three domains and design interventions targeting specific risks.
Treatment in Practice
Addiction recovery programmes increasingly adopt biopsychosocial approaches. A complete treatment plan might include:
- Medication-assisted treatment for biological stabilization
- Individual therapy for trauma processing and skill development
- Group therapy for peer support and social learning
- Family therapy to address relationship patterns
- Case management for housing, employment, and social services
This combined model represents current best practices in addiction treatment. It addresses substance use disorders from multiple angles instead of oversimplifying to one cause or solution.
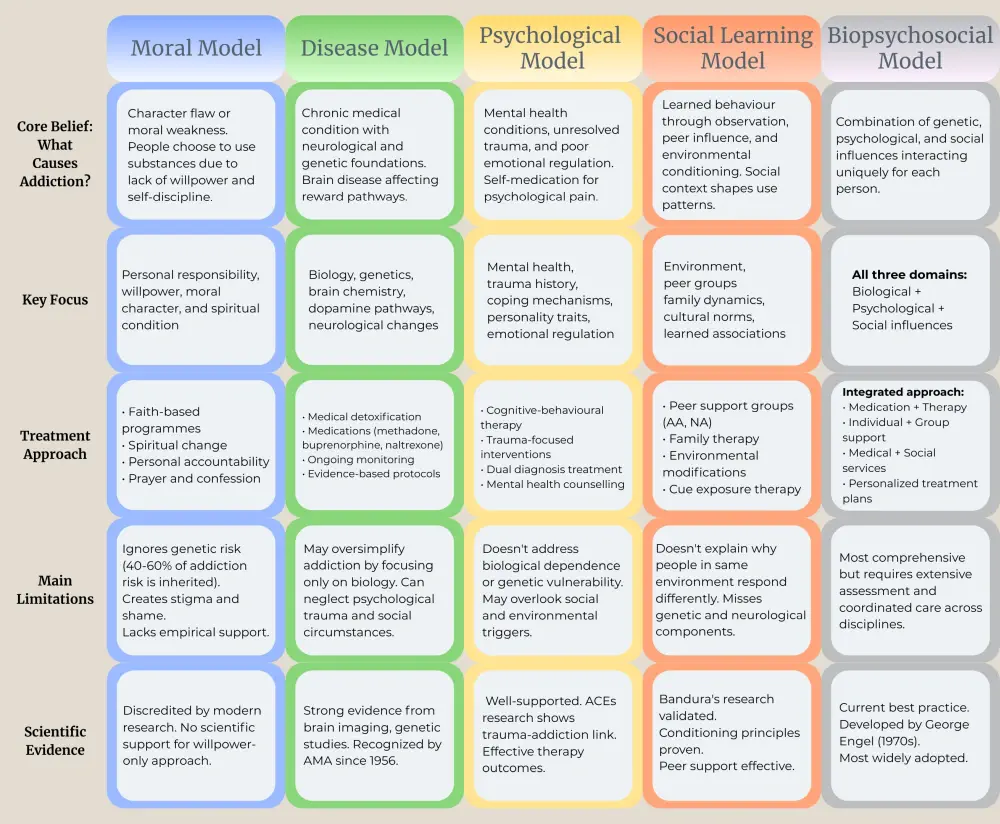
How Do Different Models Impact Treatment Approaches?
Each model directly influences treatment philosophy and methods. Knowledge of addiction models helps professionals design effective interventions.
- The moral model of addiction leads to faith-based programmes emphasizing spiritual change and personal accountability. These approaches work for some people but lack empirical support as standalone treatments.
- Disease models of addiction prioritize medical detoxification, medication management, and ongoing monitoring. Healthcare providers view relapse as symptom recurrence requiring treatment adjustment, not moral failure.
- Psychological models generate therapy-focused interventions. Counselling addresses underlying mental health conditions, teaches coping skills, and processes trauma.
- Social models create peer support networks, family therapy programmes, and community-based interventions. These approaches modify environmental influences maintaining addiction.
- The biopsychosocial model combines all these elements. Most treatment facilities today use integrated approaches instead of adhering rigidly to one framework.
Effective addiction recovery matches treatment to individual needs. Someone with severe biological dependence needs medical stabilization first. Someone whose addiction stems primarily from trauma requires psychological intervention. Most people benefit from addressing multiple dimensions simultaneously.
Which Addiction Model Should Guide Your Recovery?
Different models of addiction provide valuable perspectives on how addictive behaviours develop and persist. Historical approaches like the moral model of addiction still influence some thinking, yet addiction recovery programmes increasingly embrace evidence-based methods that consider multiple contributing influences. The most effective treatment combines medical, therapeutic, and social interventions, recognizing that each person's experience with addiction is unique and requires personalized care.
FAQ
Which model of addiction is most accurate?
No single model fully explains addiction. The biopsychosocial model offers the most complete picture because it combines biological, psychological, and social influences. Research consistently shows that addiction results from multiple interacting causes instead of one root problem.
Are disease models of addiction scientifically proven?
Yes. Brain imaging studies confirm measurable neurological changes in people with substance use disorders. Genetic research demonstrates inherited vulnerability. However, biological influences alone don't account for all cases—psychological and social dimensions also play crucial roles.
Can addiction be cured?
Most experts view addiction as a chronic condition requiring ongoing management, similar to diabetes or hypertension. People can achieve long-term recovery and live fulfilling lives, but they need continued support and vigilance instead of a one-time "cure."
Do different substances require different treatment models?
Core principles apply across substances, but specific treatments vary. Opioid addiction requires medication-assisted treatment in most cases, whereas gambling addiction (a behavioural addiction) focuses on psychological and social interventions. The biopsychosocial model adapts to different substances and behaviours.
Why do some people become addicted and others don't?
Addiction risk varies based on genetics, environment, and personal history. Someone with genetic vulnerability, childhood trauma, and peer substance use faces a higher risk than someone with protective influences like strong family support and healthy coping skills. No single risk guarantees addiction will develop; it emerges from how these influences combine for each individual.
How do I choose the right treatment approach?
Start with a professional assessment that evaluates your biological needs (withdrawal risks, co-occurring health conditions), psychological state (mental health, trauma history), and social situation (support systems, living environment). If you have severe physical dependence, medical stabilization comes first. If trauma drives your substance use, trauma-focused therapy proves crucial.
Article sources
- Agrawal, A., & Lynskey, M.T. (2008). "Are there genetic influences on addiction: Evidence from family, adoption and twin studies." Addiction, 103(7), 1069-1081. Available at: https://onlinelibrary.wiley.com/doi/10.1111/j.1360-0443.2008.02213.x
- Engel, G.L. (1977). "The need for a new medical model: A challenge for biomedicine." Science, 196(4286), 129-136. Available at: https://www.science.org/doi/10.1126/science.847460
- Volkow, N.D., Koob, G.F., & McLellan, A.T. (2016). "Neurobiologic advances from the brain disease model of addiction." New England Journal of Medicine, 374(4), 363-371. Available at: https://www.nejm.org/doi/full/10.1056/NEJMra1511480
- Bandura, A. (1977). "Social learning theory." Englewood Cliffs, NJ: Prentice Hall. Available at: https://www.worldcat.org/title/social-learning-theory/oclc/2986026
- Felitti, V.J., et al. (1998). "Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study." American Journal of Preventive Medicine, 14(4), 245-258. Available at: https://www.ajpmonline.org/article/S0749-3797(98)00017-8/fulltext
- Jellinek, E.M. (1960). The Disease Concept of Alcoholism. New Haven: Hillhouse Press. Available at: https://www.worldcat.org/title/disease-concept-of-alcoholism/oclc/395499
- Marlatt, G.A., & Baer, J.S. (1988). "Addictive behaviors: Etiology and treatment." Annual Review of Psychology, 39, 223-252. Available at: https://www.annualreviews.org/doi/10.1146/annurev.ps.39.020188.001255
- Volkow, N.D., & Morales, M. (2015). "The brain on drugs: From reward to addiction." Cell, 162(4), 712-725. Available at: https://www.cell.com/cell/fulltext/S0092-8674(15)00847-9
- Hall, W., Carter, A., & Forlini, C. (2015). "The brain disease model of addiction: Is it supported by the evidence and has it delivered on its promises?" The Lancet Psychiatry, 2(1), 105-110. Available at: https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(14)00126-6/fulltext





