We offer medical detox and multiple addiction treatment options in our
luxury treatment centres in Port Hope, Cobourg, and Ottawa.
Impulse Control in Addiction Recovery
Impulse control stands between you and relapse. Every person in addiction recovery faces moments when cravings surge without warning, when old patterns whisper promises of relief. Your ability to pause before acting, to recognize urges without surrendering to them, determines whether you move forward or slip backward.

Key Takeaway:
- Why impulses feel impossible to resist — discover the real neurological reason behind struggles that have nothing to do with willpower or character.
- Which five emotions become the most dangerous triggers — and how each one exploits a different type of brain damage to bypass your conscious control entirely.
- Seven evidence-based techniques that actually work — including the simple 10-second method that reengages your damaged decision-making centre and why it creates measurable changes in craving intensity.
- Which professional therapies repair what self-help cannot — and why certain approaches target the specific brain structures that need rebuilding during your recovery timeline.
What Happens in Your Brain When Impulse Control Breaks Down?
How Emotions Hijack Your Decision-Making
Emotional regulation connects directly to impulse management. When feelings become overwhelming (anger flaring after a difficult conversation, loneliness settling in after friends leave, anxiety spiking before an important meeting), substances once offered escape. The emotional centres of your brain learned to demand chemical relief before rational thought could intervene.
What Recovery Requires
Rebuilding impulse control demands time and deliberate practice. Research shows the brain needs three to six months before noticeable improvements emerge, with fuller recovery taking up to two years of sustained sobriety. Recognizing that urges are temporary neurological events, not commands you must obey, becomes the first step toward rewiring these damaged pathways.
What Part of Your Brain Should Stop Automatic Responses?
The prefrontal cortex acts as your brain's brake pedal for impulsive urges. This region handles planning, evaluates consequences, and weighs options before acting. Chronic substance use physically shrinks neural tissue and reduces blood flow to these critical areas.
Brain scans of people with long-term substance dependencies show measurably less grey matter in prefrontal regions compared to people without addiction histories. This isn't metaphorical damage. It's a structural change visible on imaging equipment.
How Does Each Use Session Weaken Your Self-Control Further?
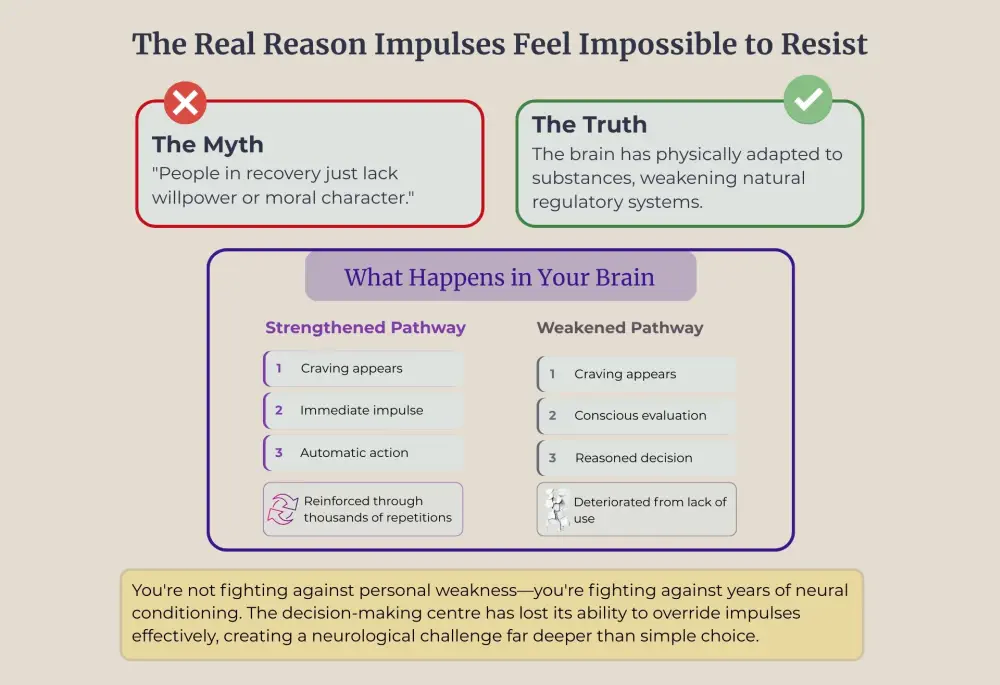
The destruction follows a predictable sequence. Each time substances flood your reward system, they reinforce pathways connecting environmental cues to substance use. Your brain interprets these repeated patterns as survival information worth prioritizing. The neurons fire together repeatedly, strengthening these connections through a process called long-term potentiation.
Simultaneously, regulatory circuits responsible for self-control weaken from disuse. When you consistently bypass conscious decision-making, when substances provide immediate relief without requiring executive function, those higher-order pathways atrophy. Your brain reallocates resources toward what gets used most: automatic stimulus-response patterns.
What's Behind the Disconnect Between Wanting and Doing?
Brain imaging reveals specific changes that explain why resisting cravings feels physically difficult beyond psychological challenges alone. The anterior cingulate cortex, which manages emotional regulation and cognitive control, shows dramatically reduced activity during tasks requiring impulse inhibition.
Your limbic system(the emotional centre) remains highly active during early recovery. It continues sending powerful signals about threats, desires, and needs. But the executive function regions that should modulate these signals struggle to exert any meaningful control. You're essentially driving a car where the gas pedal works perfectly, but the brakes barely function.
The Dopamine Problem Nobody Talks About
Dopamine dysregulation creates a vicious cycle. Substances deliver dopamine surges 2-10 times higher than natural rewards produce. Your brain compensates for this flooding by reducing receptor sensitivity, essentially turning down the volume on dopamine signals.
This adaptation means two disastrous things: everyday pleasures register as barely noticeable, creating anhedonia, and substance-related cues trigger disproportionately powerful cravings. Your brain has recalibrated itself to function in a chemical environment that no longer exists, leaving you vulnerable to impulses that promise to restore that familiar state.

How Do Emotional Triggers Exploit Your Weakened Brain?
Stress
Stress triggers impulsive substance use more frequently than any other emotional state. Cortisol release creates physical tension that evolved to prepare you for danger. But your damaged anterior cingulate cortex can't distinguish between genuine emergencies and everyday frustrations—a work deadline registers with the same neurological intensity as a life-threatening situation. Without functioning regulatory systems, your brain defaults to the quickest available relief mechanism.
Anger
The amygdala fires intensely during angry moments. That signal should travel to your prefrontal cortex for evaluation, but those pathways have weakened dramatically. Your emotional centre broadcasts distress signals that never receive regulatory input, demanding immediate discharge with no pause, no evaluation, no consideration of consequences.
Loneliness
Loneliness activates brain regions associated with physical pain—social rejection literally lights up the same neural networks as breaking a bone. Substances hijacked these connection-seeking circuits, teaching your brain that chemical relief could substitute for authentic relationships. When social situations feel threatening, your damaged reward system remembers the easier path, creating powerful impulses toward avoidance and chemical comfort.
Anxiety
The anxious brain experiences constant low-level activation that exhausts executive function resources. Your prefrontal cortex must work overtime trying to regulate persistent threat responses, but it's already damaged and weak. Eventually, it gives up, leaving impulses completely unopposed.
Depression
Depression alters dopamine signalling, creating anhedonia—the inability to experience pleasure. Combined with addiction-related receptor damage, you face a devastating double deficit where nothing brings joy. Memories surface of substances once making you feel something, creating impulses driven by desperation to escape emotional numbness rather than pleasure-seeking.

What Practical Methods Work for Controlling Impulses?
These evidence-based techniques work with your healing brain, not against it. Each exploits specific neuroscience principles to rebuild damaged regulatory systems:
⏺ The Pause Technique - Count to ten slowly when urges hit. This 10-second delay gives blood flow time to reach your weakened prefrontal cortex, allowing it to begin processing the situation. Research shows that craving intensity decreases dramatically within five minutes when people resist initial impulses. The counting also engages working memory, which competes for neural resources with craving circuits.
⏺ Environmental Distance - Remove yourself immediately from triggering locations, people, or objects. This exploits how your damaged reward system functions: strengthened pathways connecting cues to use activate automatically when environmental stimuli appear. Remove the stimuli, and the pathways can't fire. You're buying time for executive function to engage without needing to override automatic responses.
⏺ Distraction Through Activity - Exercise floods your system with endorphins and dopamine through natural pathways, temporarily satisfying depleted reward circuits. Creative activities engage prefrontal regions involved in planning and sequencing—essentially, physical therapy for injured brain tissue. Phone calls with trusted friends provide a connection that addresses loneliness-related dopamine deficits and releases oxytocin to modulate stress responses.
⏺ If-Then Planning - Create pre-formed responses during calm moments: "If I feel lonely Friday night, then I'll attend a support group." This program's replacement automatic responses don't require on-the-spot decision-making when executive function collapses. These plans become habitual through repetition, gradually replacing old impulsive patterns.
⏺ Mindfulness Practice - Learn to observe urges without reacting: "I'm having a craving, "not "I must use." This recreates the evaluation step that weakened neural pathways no longer supply automatically. Regular practice actually strengthens prefrontal cortex tissue—brain imaging shows increased grey matter density in executive function regions after eight weeks of consistent meditation.
⏺ Sleep Quality (7-9 hours nightly) - Sleep deprivation reduces prefrontal cortex activity by up to 40%. When exhausted, your already-damaged executive systems essentially shut down, leaving impulses completely unopposed. Sleep also consolidates new neural patterns you're building, making recovery behaviours more permanent.
⏺ Targeted Nutrition - Omega-3 fatty acids form brain cell membrane structures. B vitamins power neurotransmitter creation processes. Amino acids provide raw materials for dopamine, serotonin, and norepinephrine synthesis. Processed foods and sugar create energy crashes that impair executive function, while balanced meals maintain the stable blood glucose your struggling prefrontal cortex requires for operation.
How Does Professional Support Strengthen Impulse Control?
Cognitive-Behavioural Therapy (CBT)
Manually rebuilds the evaluation step that damaged prefrontal-limbic connections no longer provide. A therapist helps identify distorted thoughts like "I can't handle this without using" and systematically examines evidence, forcing activation of prefrontal regions responsible for logical analysis. Through hundreds of repetitions, you strengthen the same neural pathways that substance use weakened—creating new automatic responses involving conscious evaluation.
Dialectical Behaviour Therapy (DBT)
Provides pre-programmed responses for when executive function fails. Opposite action (doing the opposite of what impulses demand) creates alternative automatic pathways that activate even when conscious deliberation collapses. Distress tolerance skills teach specific techniques for surviving emotional intensity without chemical intervention—building the capacity damaged reward systems can no longer provide naturally.
Group Therapy
Activates mirror neuron systems that support learning through observation. Your brain processes others' experiences almost as your own, creating neural activation patterns without personal trial-and-error. Verbalizing successful techniques reinforces supporting neural pathways, while regular attendance creates external accountability that compensates for weakened internal motivation systems.

Medication When Appropriate
Addresses neurochemical imbalances directly. SSRIs increase serotonin availability, reducing emotional volatility that overwhelms damaged regulatory systems. Mood stabilizers dampen amygdala hyperactivity. Naltrexone blocks opioid receptors in reward processing circuits. These create neurochemical conditions where practicing regulatory techniques becomes possible—reducing inflammation so rehabilitation can rebuild injured tissue.
Treating Co-Occurring Conditions
Depression, anxiety disorders, ADHD, and trauma each impair executive function through distinct mechanisms. When combined with addiction-related damage, you're fighting multiple sources of impairment simultaneously. Treating underlying conditions removes additional layers of dysfunction, allowing your brain to direct limited healing resources toward addiction recovery specifically.
Long-Term Support (12-18 months minimum)
Prefrontal cortex function requires this duration for substantial improvement. You cannot rush neural tissue regeneration. Early sessions focus on crisis management when regulatory capacity barely exists. Later sessions address subtler challenges as executive function gradually returns, matching your brain's actual healing timeline.
The Canadian Centre for Addictions integrates these evidence-based therapies to target both the neurological damage and learned responses that developed during active addiction.
Our programs recognize that impulse control and emotional regulation require specialized, comprehensive support throughout the recovery timeline.
FAQ
How long does it take to rebuild impulse control after addiction?
Most people notice initial improvements within three to six months of sustained sobriety. Prefrontal cortex function shows substantial improvement between 12 to 18 months, with full recovery taking up to two years. Consistent practice of regulation techniques accelerates healing by stimulating damaged brain regions.
Can you have impulse control problems without having addiction?
Yes. Gambling disorder, compulsive shopping, and intermittent explosive disorder all involve similar prefrontal cortex dysfunction without substance dependency. These conditions share neurological patterns with addiction and respond to comparable treatments targeting weakened executive function and impaired inhibitory control circuits.
What's the difference between impulse control and willpower?
Impulse control involves measurable neurological systems that brain imaging can verify. Willpower suggests moral strength, implying personal failure when impulses win. This framing creates shame that worsens regulatory function. Brain-based understanding treats impulsive behaviour as a neurological impairment requiring rehabilitation, reducing stigma and improving outcomes.
Do certain substances damage impulse control more than others?
Stimulants like cocaine and methamphetamine create severe impulsivity through dramatic dopamine surges and direct prefrontal cortex tissue damage. Alcohol impairs decision-making through neurotoxicity, thiamine deficiency, and disrupted sleep. All dependency-forming substances alter impulse regulation systems, but stimulants and alcohol cause particularly pronounced damage.
How can family members support someone's impulse control development?
Recognize impulsive behaviour as brain injury requiring 12-24 months of healing time. Create environments with fewer triggers to compensate for regulatory deficits. Celebrate small improvements reflecting neural healing milestones. Respond to the struggling brain during difficult moments, not the person's character, maintaining emotional connection throughout the recovery timeline.
Article sources
- Volkow, N.D., et al. (2022). "Neurobiologic Advances from the Brain Disease Model of Addiction." New England Journal of Medicine, 374, 363-371. Available at: https://www.nejm.org/doi/full/10.1056/NEJMra1511480
- Koob, G.F., & Volkow, N.D. (2016). "Neurobiology of addiction: a neurocircuitry analysis." The Lancet Psychiatry, 3(8), 760-773. Available at: https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(16)00104-8
- Zilverstand, A., et al. (2018). "Neuroimaging Impaired Response Inhibition and Salience Attribution in Human Drug Addiction: A Systematic Review." Neuron, 98(5), 886-903. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC6794954/
- Gowin, J.L., et al. (2022). "Emotion regulation in substance use disorders: a systematic review and meta-analysis." Addiction, 118(1), 30-47. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC10087816/
- Eisenberger, N.I., & Lieberman, M.D. (2004). "Why rejection hurts: a common neural alarm system for physical and social pain." Trends in Cognitive Sciences, 8(7), 294-300. Available at: https://www.cell.com/trends/cognitive-sciences/fulltext/S1364-6613(04)00125-0
- Hölzel, B.K., et al. (2011). "Mindfulness practice leads to increases in regional brain gray matter density." Psychiatry Research: Neuroimaging, 191(1), 36-43. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC3004979/
- Sinha, R. (2008). "Chronic stress, drug use, and vulnerability to addiction." Annals of the New York Academy of Sciences, 1141, 105-130. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC2732004/
- Goldstein, R.Z., & Volkow, N.D. (2011). "Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications." Nature Reviews Neuroscience, 12(11), 652-669. Available at: https://www.nature.com/articles/nrn3119
- Tang, Y.Y., et al. (2015). "The neuroscience of mindfulness meditation." Nature Reviews Neuroscience, 16(4), 213-225. Available at: https://www.nature.com/articles/nrn3916





