We offer medical detox and multiple addiction treatment options in our
luxury treatment centres in Port Hope, Cobourg, and Ottawa.
7 Stages of The Addiction Cycle in 2026
About 21% of Canadians (roughly 6 million people) will meet addiction criteria during their lifetime. Recognizing the stages of addiction early enables intervention before reaching crisis stages. Each stage presents opportunities for change, though later intervention requires more intensive addiction treatment. Catching problems early makes the path forward far more manageable.
Key Takeaways:
- Stage 1: "Why first-time use doesn't automatically lead to addiction" — which specific factors determine who progresses...
- Stage 2: "How your brain forms patterns before you realize what's happening" — the subtle shift when substances move from weekend activity to daily necessity...
- Stage 3: "Why consequences stop mattering at a certain point" — see how brain changes disable your ability to recognize danger...
- Stage 4: "The critical difference between physical dependence and addiction" — why chronic pain patients aren't automatically addicted...
- Stage 5: "What happens when multiple brain systems fail simultaneously" — why willpower alone can't overcome neurological collapse...
- Stage 6: "What rock bottom actually looks like" — recognize the specific crisis events that finally break through denial...
- Stage 7: "Why recovery succeeds even after years of active addiction" — see the evidence behind the 95.6% success rate...
What is the Cycle of Addiction?
The stages of addiction describe how substance use progresses from casual experimentation to compulsive dependency through distinct, predictable stages. Your brain's reward system releases dopamine whenever you experience pleasure—eating favourite foods, spending time with loved ones, or using substances.
How Substances Hijack Your Brain's Reward System
Drugs and alcohol hijack this natural reward mechanism, flooding neural pathways with dopamine levels far beyond what normal activities produce. Over time, the brain adapts by reducing natural dopamine production and receptor sensitivity. The substance becomes necessary just to feel normal.
This neurological adaptation explains why someone can't simply "choose" to stop using. The brain has physically rewired itself around the substance. Each stage brings bigger changes in neural pathways, making reversal progressively harder without professional intervention. Recognizing these patterns of addiction helps families spot problems early and intervene before full dependency takes hold.

Stage 1: Initial Use and Experimentation
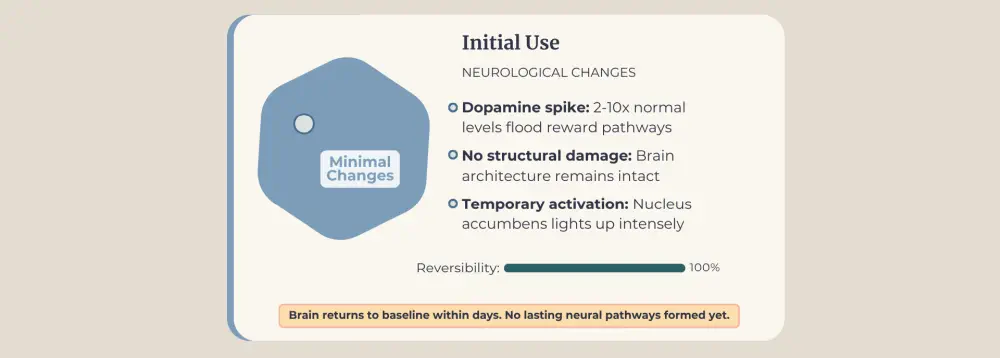
Initial use marks your first encounter with a substance through curiosity, peer pressure, or legitimate medical prescriptions. Research consistently shows that early substance use significantly increases addiction risk, with vulnerability highest when use begins during adolescence, before brain development completes around age 25.
This first experience creates pleasurable sensations the mind wants to repeat, yet a single encounter doesn't equal addiction. Many people try substances once or twice, then move on without issue. No pattern has formed yet.
Experimentation means testing substances in different contexts—teenagers drinking at parties to feel more confident, young adults trying cannabis to manage stress. The behaviour remains sporadic and situational. Quitting feels easy because the brain hasn't yet formed strong associations between substances and daily routines.
What Determines Who Progresses
Several factors determine whether experimentation progresses: genetic predisposition increases vulnerability, existing mental health conditions create motivation for self-medication, environments normalizing substance use remove barriers, early age of first use interferes with development, and certain substance types prove more addictive. Red flags include increased frequency, defensive reactions when questioned, and planning activities around substance availability. The substance abuse cycle begins here, at a point where intervention can prevent everything that follows.
Stage 2: Regular Use Develops Into a Pattern
Regular use emerges when substances transform from occasional choices into expected routines. That nightly glass of wine to unwind becomes non-negotiable. Weekend cannabis experimentation shifts to a daily ritual. Your brain begins anticipating the substance at specific times, forging neural pathways connecting environmental cues, getting home from work, finishing dinner, weekend evenings, directly to substance use.
Tolerance starts its insidious work. The dose that initially delivered desired effects now barely registers. Your brain compensates for regular substance presence by downregulating receptors, requiring more substance to achieve the same result. Meanwhile, life impacts begin surfacing—chronically showing up late to work, nursing hangovers, productivity declining, and relationships showing strain from missed commitments.
The Mind Convinces Itself Before the Body Does
Mental dependence emerges before any physical addiction takes root. Your mind insists substances help you cope with stress, improve social situations, or simply make life bearable. The brain manufactures increasingly elaborate justifications for established habits despite mounting evidence suggesting otherwise. You're not physically sick without the substance yet, but psychologically? You've already concluded you need it.
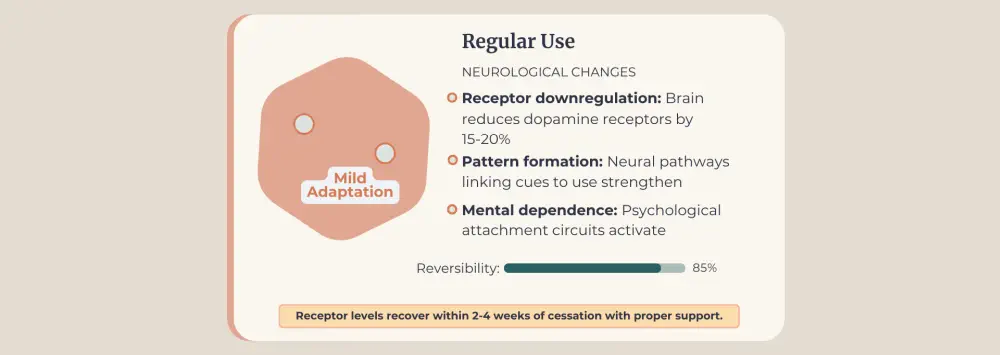
Why This Stage Offers Excellent Treatment Outcomes
Intervention during regular use yields excellent outcomes precisely because physical dependence hasn't developed. Outpatient therapy successfully helps people identify specific triggers and develop healthier coping mechanisms. Understanding various types of addiction reveals that this pattern-formation stage affects multiple substance categories similarly, though each brings unique challenges requiring tailored therapeutic responses.
Stage 3: Risky Use Escalates Despite Consequences
Risky use marks the stage where consequences pile up yet somehow fail to change behaviour. Driving under the influence starts feeling normal. Missing work or showing up high seems acceptable. Behaviours you'd never have considered before become routine. What's different here from earlier stages? Your brain has lost the ability to properly evaluate danger.
The prefrontal cortex(your decision-making headquarters) now shows measurable impairment from repeated substance exposure. Risk versus reward calculations that once protected you have broken down. This isn't moral weakness or poor character; it's compromised neurobiology making sound judgment neurologically impossible.
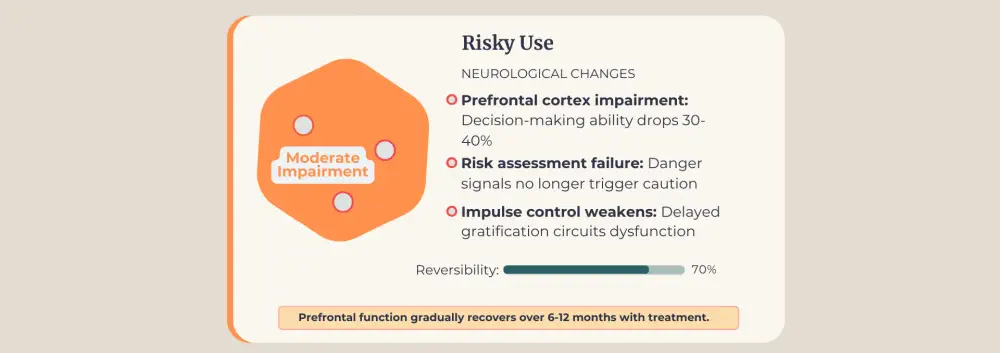
Relationships actively deteriorate around you. Family members stage confrontations about behaviour changes. Partners deliver ultimatums. Work or school performance metrics drop measurably. Money designated for bills flows toward substances instead, creating financial chaos. Legal problems materialize—DUI arrests, possession charges, and court dates multiply.
Physical health warnings emerge from doctors concerned about liver function or blood pressure readings. The gap between how you perceive your situation and objective reality widens into a chasm. You maintain that use remains "under control" even as everyone else watches your life unravel in real-time.
The Final Window for Less Intensive Help
Professional intervention grows increasingly critical. Outpatient programs might still succeed here, though many people require more structured environments addressing the deeper issues driving continued use. This stage represents the final window where less intensive interventions can work. Once physical dependence takes hold, the treatment requirements escalate dramatically.
Stage 4: Physical Dependence Takes Hold
Physical dependence develops when your body adapts so completely to substance presence that stopping produces measurable withdrawal symptoms. The brain has restructured baseline chemistry around the substance. What once created pleasure now simply prevents suffering. The substance isn't for getting high anymore; it's for avoiding withdrawal hell.
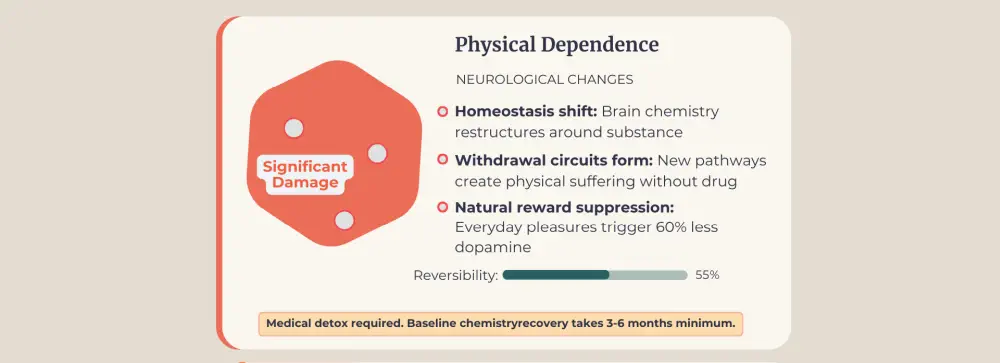
How Withdrawal Differs by Substance
Alcohol tolerance and dependence create tremors, sweating, nausea, anxiety, and potentially life-threatening seizures. Opioid withdrawal produces intense muscle aches and severe gastrointestinal symptoms. Stimulant withdrawal primarily affects mood—deep depression, anhedonia, and extreme fatigue.
Physical dependence doesn't automatically mean addiction. Someone taking prescribed opioids for chronic pain becomes physically dependent but isn't addicted if they use the medication as directed without compulsive patterns. Dependence crosses into addiction territory when substances are used compulsively despite mounting harm.
Your entire day now centers on ensuring substance availability. You plan meticulously to never run out. Running low triggers genuine panic. Relationships fracture as partners leave and family members create distance. Employment situations deteriorate toward termination if jobs haven't already been lost.
Why Medical Detox Becomes Non-Negotiable
Medical detoxification becomes necessary rather than optional. Stopping certain substances without medical supervision can kill you. Professional detox programs provide medications to ease withdrawal symptoms, monitor vital signs, and prevent dangerous complications. This medically supervised transition represents recovery beginning, not its endpoint—physical stabilization merely creates conditions for psychological healing to begin.
Stage 5: Full Addiction and Complete Control Loss
Full addiction represents complete control loss—substances dictate every decision, every priority, every waking moment. What separates this from physical dependence? Multiple brain systems have now failed simultaneously.
Brain imaging reveals the scope: reduced prefrontal cortex activity destroys judgment, hyperactive amygdala manufactures constant stress responses, and the nucleus accumbens shows blunted responses to natural pleasures while remaining hypersensitive to substance cues.

You use despite desperately wanting to stop. Every promise to yourself about cutting back crumbles. Substances consume everything—jobs vanish, relationships disintegrate, housing disappears. Mental health collapses as depression and anxiety disorders take root alongside addiction, each condition feeding the other in destructive cycles.
How Tolerance Reaches Deadly Levels
Tolerance reaches levels that defy logic. Doses that would kill someone without tolerance barely achieve baseline functioning for you. Withdrawal symptoms don't just cause discomfort—they create medical emergencies demanding immediate intervention.
What Treatment is Required at This Stage
Treatment for drug addicts requires simultaneous medical, psychological, and social interventions addressing the catastrophic damage across all life domains. Residential programs provide structured environments where clients rebuild basic coping skills from scratch. Medication-assisted treatment stabilizes disrupted brain chemistry, creating neurological conditions that allow psychological work to progress. Therapy excavates buried trauma, teaches practical coping mechanisms, and gradually reconstructs shattered self-worth.
Support extends indefinitely beyond initial treatment. Addiction operates as a chronic condition requiring lifelong management, comparable to diabetes or heart disease. Sustained recovery becomes achievable through persistent engagement with support systems, though success demands ongoing effort and commitment rather than arriving as a permanent destination.
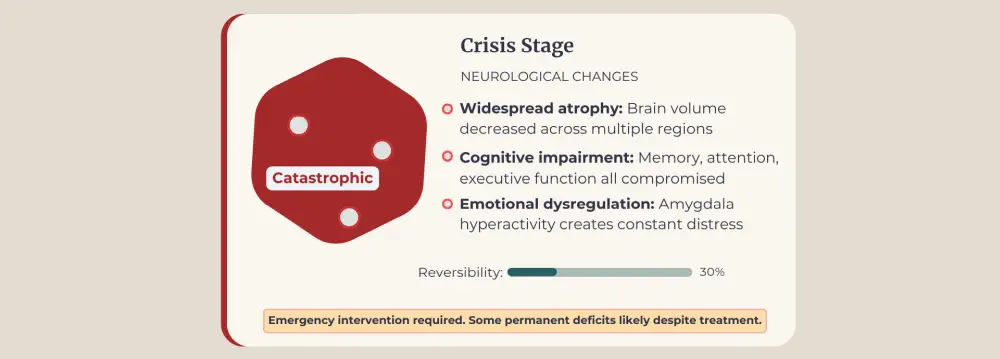
Stage 6: Crisis Stage and Rock Bottom
The crisis stage occurs when addiction consequences become so severe that they can no longer be ignored. This might involve overdose, arrest, medical emergency, loss of custody, homelessness, or devastating recognition that you can't continue this way.
Health emergencies frequently precipitate a crisis. Overdoses requiring emergency intervention shock families. Heart attacks, strokes, or organ damage create urgent situations.
- Legal consequences escalate: multiple DUI arrests, incarceration, mandated treatment.
- Financial devastation reaches critical mass: eviction, bankruptcy, and inability to meet basic needs.
Stage 7: Recovery and Treatment Path
Professional intervention becomes critical when a crisis hits. Intensive treatment addresses the catastrophic damage across all life domains while providing hope that recovery remains possible at any stage.
What Intensive Treatment Looks Like
Addiction treatment at this stage requires intensive intervention. Medical detoxification happens first, clearing substances while managing withdrawal symptoms safely. Residential programs remove people from triggering environments. Treatment duration ranges from 30 days to several months, depending on severity.
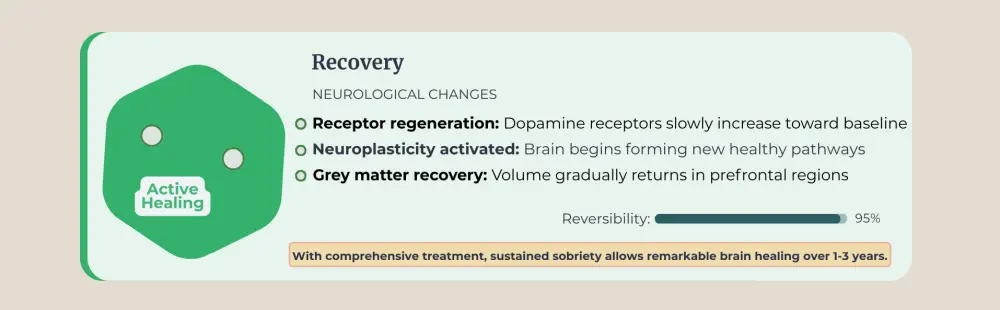
Psychological care addresses underlying issues. Trauma therapy helps work through past experiences. Depression and anxiety receive appropriate treatment through counselling and sometimes medication. Life skills training rebuilds practical capabilities supporting sobriety. Family involvement helps loved ones see addiction as a brain disease rather than a moral failure.
Why Hope Remains at Every Stage
Between January 2016 and June 2024, Canada saw 49,105 opioid toxicity deaths. Yet thousands in recovery demonstrate that lives can be rebuilt even after years of active addiction. Professional addiction treatment combined with personal commitment creates pathways from crisis to renewal. The work requires courage and time, yet recovery proves possible when proper support systems exist.
FAQ
Can you skip stages in addiction?
Individual experiences vary considerably. Some people, particularly those using highly addictive substances like fentanyl, move through stages rapidly, appearing to skip steps. Others remain in early stages for years. Genetic factors, mental health conditions, substance type, and environment all affect progression speed.
How long does each stage last?
Stage duration varies enormously. Someone might experiment for years without progressing, while another develops dependence within weeks. Highly addictive substances accelerate progression. Adolescent brains show higher vulnerability, potentially shortening timelines compared to adult-onset use.
What are the warning signs someone is progressing to the next stage?
Watch for increased frequency of use, escalating doses, defensive reactions when questioned, declining performance at work or school, withdrawing from family and friends, financial problems from substance spending, and physical changes like weight loss or neglected appearance. The gap between their self-perception and reality is widening, indicating serious progression.
Can someone recover without professional treatment?
Recovery without professional support proves extremely difficult and dangerous, particularly beyond the experimentation stage. Physical dependence creates withdrawal symptoms that can be life-threatening without medical supervision. Psychological aspects require specialized therapy addressing underlying issues.
Is addiction reversible?
Yes, brain changes can heal through neuroplasticity, though recovery takes time and professional support. Addiction creates lasting vulnerabilities, but with appropriate treatment and continued support, sustained recovery proves entirely achievable.
How can families help during each stage?
Support approaches differ by stage. At the dependence and addiction stages, families benefit from their own therapy to learn about codependency, establish boundaries, and support recovery without enabling use.
Article sources
- Statistics Canada. (2012). "Canadian Community Health Survey - Mental Health (CCHS-MH)." Government of Canada. Available at: https://www150.statcan.gc.ca/n1/daily-quotidien/130918/dq130918a-eng.htm
- Health Canada. (2024). "Opioid- and Stimulant-related Harms in Canada." Public Health Agency of Canada, December 2024 update. Available at: https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/
- Chambers, R.A., Taylor, J.R., & Potenza, M.N. (2003). "Developmental neurocircuitry of motivation in adolescence: a critical period of addiction vulnerability." American Journal of Psychiatry, 160(6), 1041-1052. Available at: https://pubmed.ncbi.nlm.nih.gov/12777258/
- Volkow, N.D., Koob, G.F., & McLellan, A.T. (2016). "Neurobiologic Advances from the Brain Disease Model of Addiction." New England Journal of Medicine, 374(4), 363-371. Available at: https://www.nejm.org/doi/full/10.1056/NEJMra1511480
- Koob, G.F., & Volkow, N.D. (2016). "Neurobiology of addiction: a neurocircuitry analysis." The Lancet Psychiatry, 3(8), 760-773. Available at: https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(16)00104-8/fulltext
- Goldstein, R.Z., & Volkow, N.D. (2011). "Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications." Nature Reviews Neuroscience, 12(11), 652-669. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3462342/
- Nutt, D.J., King, L.A., & Phillips, L.D. (2010). "Drug harms in the UK: a multicriteria decision analysis." The Lancet, 376(9752), 1558-1565. Available at: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(10)61462-6/fulltext
- Dennis, M., & Scott, C.K. (2007). "Managing addiction as a chronic condition." Addiction Science & Clinical Practice, 4(1), 45-55. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2797101/





