We offer medical detox and multiple addiction treatment options in our
luxury treatment centres in Port Hope, Cobourg, and Ottawa.
How Effective Is Opioid Agonist Therapy?
Canada faces roughly 20 opioid-related deaths daily. Families watch loved ones disappear into dependency while communities scramble for solutions that actually work. Opioid agonist therapy (OAT) stands out as the most evidence-backed intervention available, yet many people still question whether medication-based treatment truly delivers results.
The numbers tell a compelling story. Research shows this approach cuts mortality rates in half for individuals with opioid use disorder. But effectiveness extends far beyond just staying alive. Careers get rebuilt, relationships restore themselves, and futures that addiction had stolen become possible again.
Key Takeaways:
- The Science: Medications work by occupying brain receptors for 24-36 hours without creating euphoria, breaking the cycle of craving that drives repeated use
- Life-Saving Impact: Death risk drops by 50% across all causes—not just overdoses—with protection extending to suicide, cardiovascular disease, and infections
- Retention Reality: While traditional programs struggle with dropout rates, virtual delivery models achieve 90% retention at six months by removing access barriers
- Recovery Timeline: Physical relief starts within hours, but employment gains take 2-6 months, and family reconnection often requires 3-12 months of stability
- Program Variables: Reaching therapeutic dose quickly matters more than any other factor—people at proper levels show an eight-fold increase in staying with treatment
How Does Opioid Agonist Therapy Stop Cravings?
Your brain develops physical dependence on opioids through changes in its chemistry. Short-acting drugs like fentanyl or heroin create intense highs followed by crashes that drive relentless craving cycles. Opioid agonist therapy breaks this pattern using medications that act slowly and steadily.
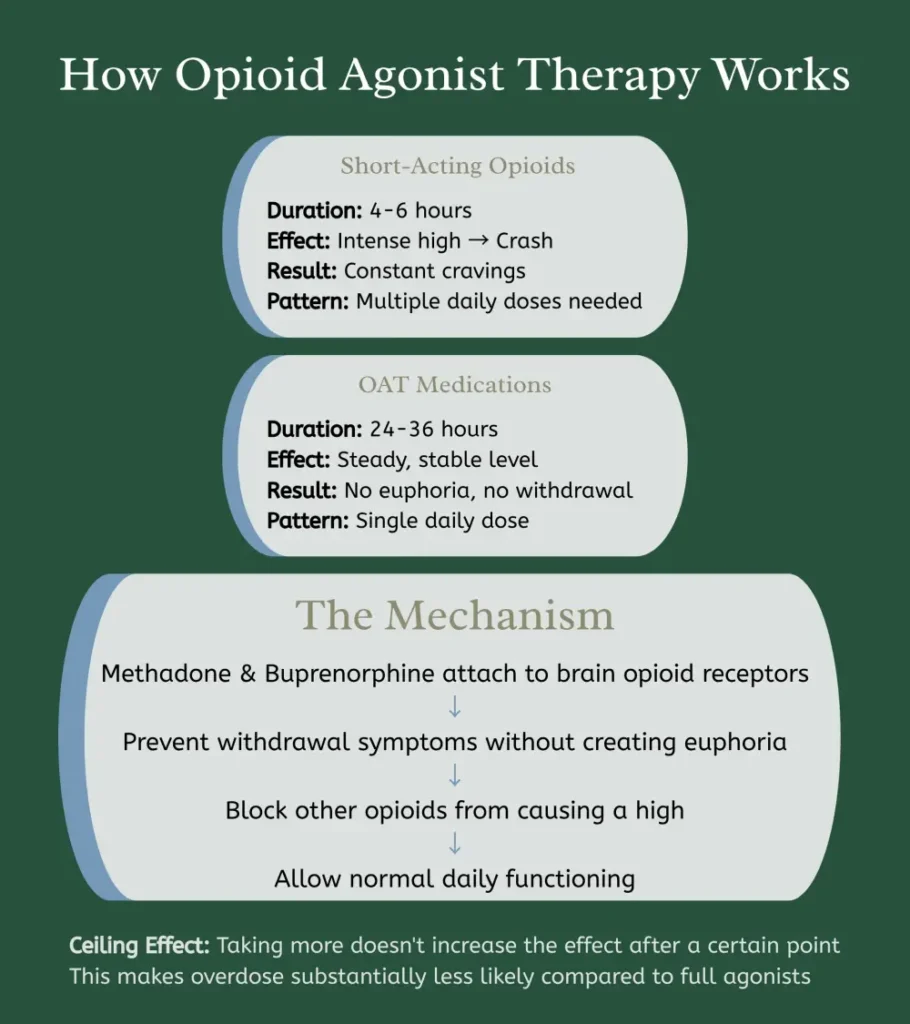
Methadone and buprenorphine attach to the same brain receptors as other opioids. They prevent withdrawal symptoms without creating euphoria. Think of them as filling a lock without turning it – they occupy the space but don't trigger the high.
The medications last 24 to 36 hours in your system. You take a single daily dose and function normally throughout the day. No desperate mid-day searches for relief. No withdrawal symptoms disrupting work or family time.
Buprenorphine offers unique safety features. It has a ceiling effect – taking more doesn't increase the effect after a certain point. This makes overdose less likely compared to full agonists like methadone. Many doctors prefer starting patients on buprenorphine for this reason.
Different people respond better to different medications. Some stabilise quickly on methadone while others do better with buprenorphine. The right fit often requires trying both options under medical guidance. An effective opioid treatment program personalizes medication choice to individual needs.
Does Opioid Agonist Therapy Save Lives?
Studies tracking hundreds of thousands of participants show opioid agonist therapy reduces death risk by half. This includes not just overdose deaths but mortality from all causes – suicide, cardiovascular disease, and infections.
Research published in JAMA Psychiatry analyzed data from multiple countries. Those enrolled in treatment showed substantially lower death rates compared to individuals attempting recovery without medication support. The protective effect remained strong even among those who continued using other substances occasionally.
During Canada's fentanyl crisis, communities with better opioid agonist therapy access experienced fewer overdose deaths. British Columbia data revealed people receiving treatment were substantially less likely to die during the province's worst overdose years.
Beyond preventing death, the therapy stops the health deterioration common in active addiction:
- HIV and Hepatitis C transmission drops significantly
- Emergency department visits become less frequent
- Hospital admissions for infection-related complications decrease markedly
- Overall health metrics improve across the board
Studies from Ontario found that individuals in opioid rehab programs accessing this treatment showed better outcomes in every area measured. The medication creates stability that allows healing to begin.

What Are the Retention Rates for OAT Programs?
Retention tells the real story of treatment effectiveness. Less than 30% of people with opioid use disorder typically start opioid agonist therapy, and fewer than half remain beyond six months in traditional settings. These numbers initially seem discouraging.
Recent Canadian research reveals more promising patterns. Alberta's Virtual Opioid Dependency Program achieved 90% retention at six months and 58% at one year. Virtual delivery removed barriers like transportation and scheduling conflicts that often derail treatment.
Comparing Methadone and Buprenorphine Retention
Nova Scotia data comparing methadone and buprenorphine showed that methadone patients stayed longer in treatment. Median retention reached 89 days for methadone versus 55 days for buprenorphine among those receiving daily witnessed dosing. Younger patients (under 25) faced particular challenges, averaging just 37 days on buprenorphine and 69 days on methadone.
Why Proper Dosing Matters Most
Achieving a therapeutic dose matters enormously for retention. British Columbia study found that individuals reaching adequate medication levels experienced an eight-fold increase in staying with treatment. Proper dosing – at least 60mg daily for methadone or 12mg for buprenorphine – made the difference between giving up and pushing through.
Injectable opioid agonist therapy options show retention rates as high as 70-94% at one year. These medications work for people who haven't succeeded with oral formulations. Access remains limited, but outcomes demonstrate what's possible with adequate resources.

How Will OAT Change Your Daily Life?
Quality of life improvements surprise many people starting treatment. The benefits extend across multiple life domains, each following its own recovery timeline:
| Life Area | Timeline | Specific Improvements |
|---|---|---|
| Physical Health | 1-4 weeks | Craving intensity decreases; sleep patterns normalize; energy levels return gradually |
| Mental Clarity | 2-6 weeks | Cognitive fog lifts; decision-making improves; concentration strengthens |
| Employment | 2-6 months | Return to work; job retention improves; professional skills rebuild |
| Family Relationships | 3-12 months | Custody restoration; marriages stabilize; reconnection with estranged relatives |
| Mental Health | Ongoing | Depression symptoms decrease; anxiety reduces; emotional stability returns |
| Social Functioning | 6+ months | Financial management resumes; housing stabilizes; Community participation increases |
Research tracking individuals over multiple years found that most people view their treatment as life-changing. They describe getting themselves back – the person they were before addiction took over.
What Makes an OAT Program Successful?
Several factors separate successful programs from struggling ones:
Dosing Approach
Many clinics start patients too low and increase slowly out of excessive caution. This leaves people in prolonged withdrawal, driving them back to street drugs. Reaching the therapeutic dose quickly makes the difference.
Medication Flexibility
When methadone doesn't work, switching to buprenorphine or morphine gives people alternatives rather than watching them leave treatment entirely.
Combined Services
Opioid agonist therapy paired with counselling, housing support, and vocational services produces better long-term results than medication alone. That said, medication should never be withheld from people who can't access or don't want additional services immediately.
Take-Home Options
Daily witnessed dosing works for some but creates insurmountable barriers for others. Programs allowing earned take-home doses see improved retention while maintaining safety.
Access Solutions
Rural access remains challenging. Telemedicine options show promise, with some virtual programs matching or exceeding in-person retention rates. Technology removes geography as a barrier to effective opioid rehab.
When Should You Consider Opioid Agonist Therapy?
Anyone experiencing opioid use disorder who wants to stop or reduce use should consider this option. Age, drug use duration, or previous treatment failures don't disqualify you. The medications work regardless of how long you've been using them or what you've tried before.
Access in Ontario happens through specialized clinics, primary care physicians, or some emergency departments. The Canadian Centre for Addictions in Port Hope and Cobourg provides a thorough assessment and connection to appropriate opioid treatment program resources.
Intake involves medical history review, substance use assessment, and discussion of treatment goals. Some people aim for complete abstinence, while others focus on harm reduction. Both approaches work when treatment plans respect individual goals.
Starting treatment typically happens quickly once you connect with providers. Medication begins within days rather than weeks for most patients. The sooner treatment starts, the sooner relief arrives.
FAQ
How long does OAT take to work?
Most people feel relief from withdrawal within the first dose. Complete stabilization usually requires 2-4 weeks as doctors adjust to find your therapeutic level. Cravings decrease gradually over the first month.
Is OAT just replacing one addiction with another?
No. The medications don't produce euphoria or impairment at therapeutic doses. They restore normal brain function disrupted by addiction, similar to how insulin treats diabetes. You can work, drive, and function normally.
Can I stop OAT once I start?
Yes, though most people benefit from longer treatment periods. Research shows that staying on medication for at least one year produces better outcomes. When you're ready to stop, doctors taper the dosage gradually to prevent withdrawal.
Does insurance cover treatment?
Most private insurance plans cover opioid agonist therapy medications. Ontario's public drug program provides coverage for eligible residents. The Canadian Centre for Addictions helps navigate insurance questions and find affordable treatment options.
What if the medication doesn't work for me?
Not responding to one medication doesn't mean treatment has failed. Your doctor can adjust dosages, switch between methadone and buprenorphine, or try alternatives like slow-release oral morphine. Injectable options exist for people who haven't succeeded with oral medications.
Article sources
- Santo, T., et al. (2021). "Association of Opioid Agonist Treatment with All-Cause Mortality and Specific Causes of Death Among People with Opioid Dependence: A Systematic Review and Meta-analysis." JAMA Psychiatry. Available at: https://pubmed.ncbi.nlm.nih.gov/34009271/
- Yazdani, K., et al. (2023). "Characterizing Opioid Agonist Therapy Uptake and Factors Associated with Treatment Retention Among People with HIV in British Columbia, Canada." Preventive Medicine Reports. Available at: https://pubmed.ncbi.nlm.nih.gov/37519440/
- Kirkland, S., et al. (2022). "Virtual Opioid Agonist Treatment: Alberta's Virtual Opioid Dependency Program and Outcomes." Addiction Science & Clinical Practice. Available at: https://ascpjournal.biomedcentral.com/articles/10.1186/s13722-022-00323-4
- Al-Nasseri, N., et al. (2022). "Treatment Retention in Opioid Agonist Therapy: Comparison of Methadone Versus Buprenorphine/Naloxone by Analysis of Daily-Witnessed Dispensed Medication in a Canadian Province." BMC Psychiatry. Available at: https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-022-04175-9
- Morin, K.A., et al. (2020). "Evaluating the Effectiveness of Concurrent Opioid Agonist Treatment and Physician-Based Mental Health Services for Patients with Mental Disorders in Ontario, Canada." PLOS ONE. Available at: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0243317
- Bozinoff, N., et al. (2024). "Opioid Agonist Treatment Outcomes Among Individuals with a History of Nonfatal Overdose: Findings from a Pragmatic, Pan-Canadian, Randomized Control Trial." American Journal on Addictions. Available at: https://pubmed.ncbi.nlm.nih.gov/39127891/
- Sordo, L., et al. (2017). "Mortality Risk During and After Opioid Substitution Treatment: Systematic Review and Meta-analysis of Cohort Studies." BMJ. Available at: https://www.bmj.com/content/357/bmj.j1550
- Golan, O.K., et al. (2022). "Systematic Review and Meta-analysis of Changes in Quality of Life Following Initiation of Buprenorphine for Opioid Use Disorder." Drug and Alcohol Dependence. Available at: https://pubmed.ncbi.nlm.nih.gov/35395595/
- Moazen-Zadeh, E., et al. (2021). "Impact of Opioid Agonist Treatment on Mental Health in Patients with Opioid Use Disorder: A Systematic Review and Network Meta-analysis of Randomized Clinical Trials." American Journal of Drug and Alcohol Abuse. Available at: https://pubmed.ncbi.nlm.nih.gov/33870850/
- Health Canada. (2024). "Opioid Use Disorder and Treatment." Available at: https://www.canada.ca/en/health-canada/services/opioids/opioids-use-disorder-treatment.html
- Mendell, A., et al. (2023). "Utilization of Opioid Agonist Therapies in Canada: CADTH Health Technology Review." Available at: https://www.ncbi.nlm.nih.gov/books/NBK596749/
- Canadian Research Initiative in Substance Misuse. (2024). "Management of Opioid Use Disorder: 2024 Update to the National Clinical Practice Guideline." CMAJ. Available at: https://www.cmaj.ca/content/196/38/E1280
- Ferraro, C.F., et al. (2021). "Association Between Opioid Agonist Therapy Use and HIV Testing Uptake Among People Who Have Recently Injected Drugs: A Systematic Review and Meta-analysis." Addiction. Available at: https://pubmed.ncbi.nlm.nih.gov/33150625/
- Palmateer, N., et al. (2022). "Interventions to Prevent HIV and Hepatitis C Among People Who Inject Drugs: Latest Evidence of Effectiveness from a Systematic Review (2011 to 2020)." International Journal on Drug Policy. Available at: https://pubmed.ncbi.nlm.nih.gov/36113333/
- Socias, M.E., et al. (2020). "Trajectories of Retention in Opioid Agonist Therapy in a Canadian Setting." International Journal of Drug Policy. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7577708/






