We offer medical detox and multiple addiction treatment options in our
luxury treatment centres in Port Hope, Cobourg, and Ottawa.
Burnout Recovery Stages in Addiction
Burnout recovery stages follow three clear phases: recognition, rebuilding, and resilience. Most people experience meaningful improvement within 3-12 months, though the timeline varies based on severity and how quickly you implement changes. Each phase addresses different challenges specific to addiction recovery.

Staying sober demands constant vigilance. Your body and mind need rest to heal from substance use, yet the daily requirements(attending meetings, managing triggers, rebuilding relationships) drain whatever energy remains. This creates a dangerous cycle where chronic fatigue makes maintaining sobriety feel impossible on some days.
Key Takeaways
- How burnout develops differently at 0-3 months versus 6+ months into recovery—and why late-stage exhaustion often gets mistaken for complacency when it's actually dangerous depletion
- The three essential phases you must move through to recover: recognition (2-4 weeks), active rebuilding (2-6 months), and resilience building (6+ months ongoing)
- Which recovery activities drain energy versus which actually help—and the honest evaluation framework that prevents obligation-based attendance from worsening burnout syndrome
- Why does exhaustion dramatically increase relapse risk by depleting the mental resources needed to resist cravings and making substance use look like a reasonable solution
- Specific daily practices that prevent escalation—morning energy checks, afternoon maintenance strategies, and evening recovery protocols that protect against future episodes
- How to communicate with your treatment team using concrete symptoms and timelines rather than vague complaints, so they can distinguish between chronic fatigue requiring intervention and temporary tiredness
How Does Burnout Syndrome Develop During Addiction Recovery?
Accumulated stress specific to recovery builds gradually into burnout syndrome. Constant self-monitoring for relapse warning signs becomes mentally exhausting. Every social situation requires careful planning. Sleep remains disrupted for months. Brain chemistry is still rebalancing from years of substance use.
This sustained pressure creates feelings of emotional exhaustion that rest alone won't fix. Waking up tired becomes the norm. Simple decisions feel overwhelming. The initial enthusiasm about getting clean fades into a grey numbness that frightens people back into old patterns.
The recovery process demands relentless effort across multiple fronts. Relearning stress management without substances. Repairing damaged relationships. Dealing with legal or financial wreckage. Finding new friends who support sobriety. Building a completely different life from scratch—each task requires energy that simply doesn't exist.
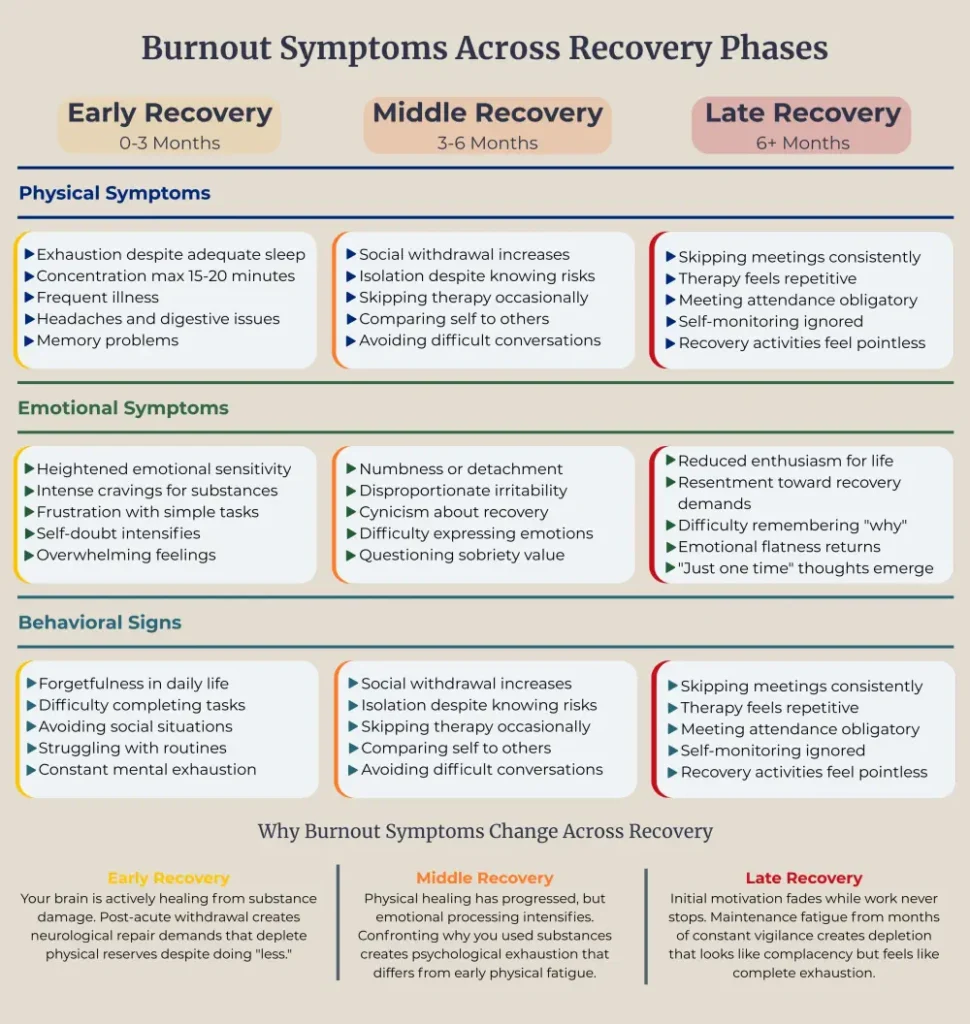
How Does Burnout Manifest During Early Recovery (0-3 Months)?
The first three months of sobriety bring unique exhaustion patterns. Your brain is actively healing from substance damage. Post-acute withdrawal syndrome creates symptoms that mimic complete depletion but stem from neurological repair. Concentration difficulties make simple tasks feel impossible. Memory problems cause frustration and self-doubt.
Physical healing demands enormous energy. Your liver regenerates cells. Your cardiovascular system recalibrates. Sleep architecture slowly normalizes after months or years of disruption. This biological restoration process depletes physical reserves, leaving you feeling drained despite doing "less" than before.
Many mistake these early symptoms for personal weakness. They're not. Your body is performing intensive internal repairs that require massive energy expenditure. This biological reality makes early recovery particularly vulnerable to developing burnout syndrome.

What Symptoms Emerge During Middle Recovery (3-6 Months)?
Months three through six bring different challenges. Physical healing has progressed, but emotional processing intensifies. You're confronting why you used substances in the first place. This psychological work creates its own form of exhaustion.
Therapy sessions unearth painful memories. Relationship repair conversations drain emotional reserves. Grief for time lost to addiction surfaces unexpectedly. Guilt and shame about past actions require constant mental processing. This emotional labour exhausts people in ways physical work never could.
This phase also brings comparison fatigue. Seeing others succeed in areas where you're still struggling creates demoralization. Social media shows people thriving months into recovery. Your reality feels messier, harder. This discrepancy between expectations and experience fuels burnout syndrome.
How Does Burnout Present During Late Recovery (6+ Months)?
Six months and beyond introduce maintenance fatigue. The initial motivation that carried you through early sobriety has faded. Recovery has become routine, but routines require sustained energy. The novelty of sobriety has worn off, yet the work never stops.Late recovery chronic fatigue often looks like complacency but feels different internally. You're not giving up — you're simply depleted from months of vigilance. Meeting attendance feels obligatory rather than supportive. Therapy sessions seem repetitive. The constant self-monitoring becomes background noise you're tempted to ignore.
Stage One: Recognition & Acknowledgement
Recognition starts when denial finally breaks. This usually takes 2-4 weeks after symptoms begin, though some push through denial much longer. The realization hits that what's happening goes beyond normal recovery challenges.
Acknowledgement means accepting that powering through alone won't work. Many resist this stage, fearing others will view them as weak or uncommitted. After working so hard to stay clean, admitting struggle feels like failure.
The stages of recovering from burnout can't begin without stopping the pretense that everything's fine. Tell your sponsor, therapist, or trusted friend what's actually happening. Writing down symptoms helps reveal patterns previously dismissed.
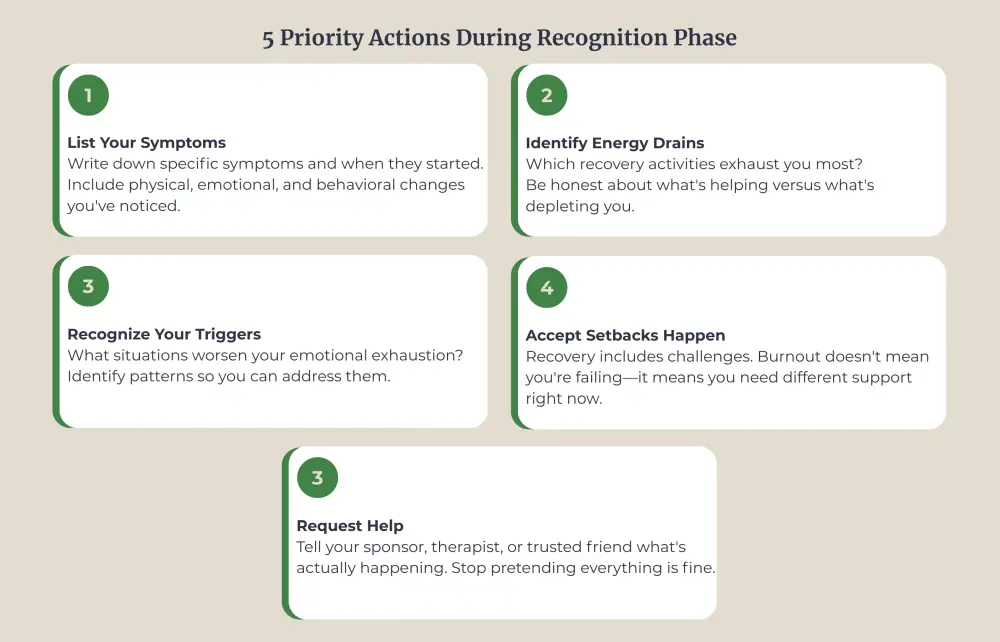
Rest becomes non-negotiable. Cancel non-mandatory obligations. Primary focus shifts from perfection to basic self-preservation. Sleep, eat, hydrate. These sound simple, but chronic fatigue makes even basic self-care feel monumental.
Stage Two: Active Rebuilding
Active rebuilding typically spans 2-6 months after the problem is acknowledged. This phase requires concrete changes to how recovery is approached. Doing everything the same way while expecting different results won't work.
Start by examining which recovery activities actually help versus which are done out of obligation. Attending meetings seven days a week might prove counterproductive if exhaustion prevents absorbing anything. Quality matters more than quantity.
Create boundaries around time and energy. Learn to decline requests that deplete without genuine benefit. Skip some social events. Reduce work hours temporarily. Step back from volunteer commitments. Burnout syndrome thrives on perfectionism and unrealistic expectations. Staying clean today is enough—no superstar performance required.
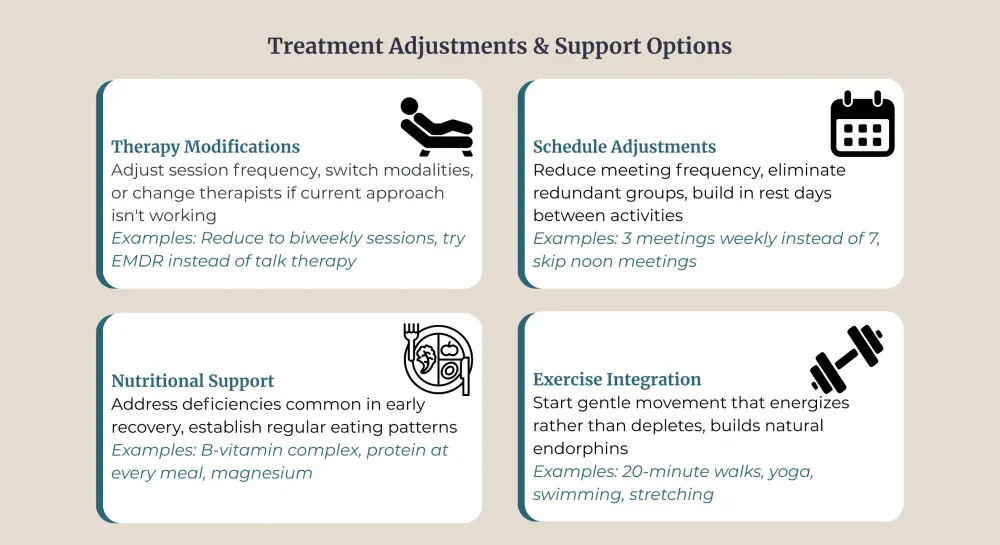
Professional support proves invaluable here. Therapists experienced with helping people stay sober help distinguish between healthy practices and behaviours that fuel exhaustion. They provide a perspective impossible to maintain when too close to the situation.
Support systems need education about what's happening. People who care might not recognize that this exhaustion differs from normal fatigue. Explain that burnout syndrome requires specific interventions, not just "trying harder" or "staying positive."
Stage Three: Resilience Building
Resilience building starts around month 6 and continues indefinitely. Changes have been implemented, and improvement has started. Now the work shifts to maintaining those gains and preventing future episodes.
This phase teaches recognition of early warning signs before full depletion develops.
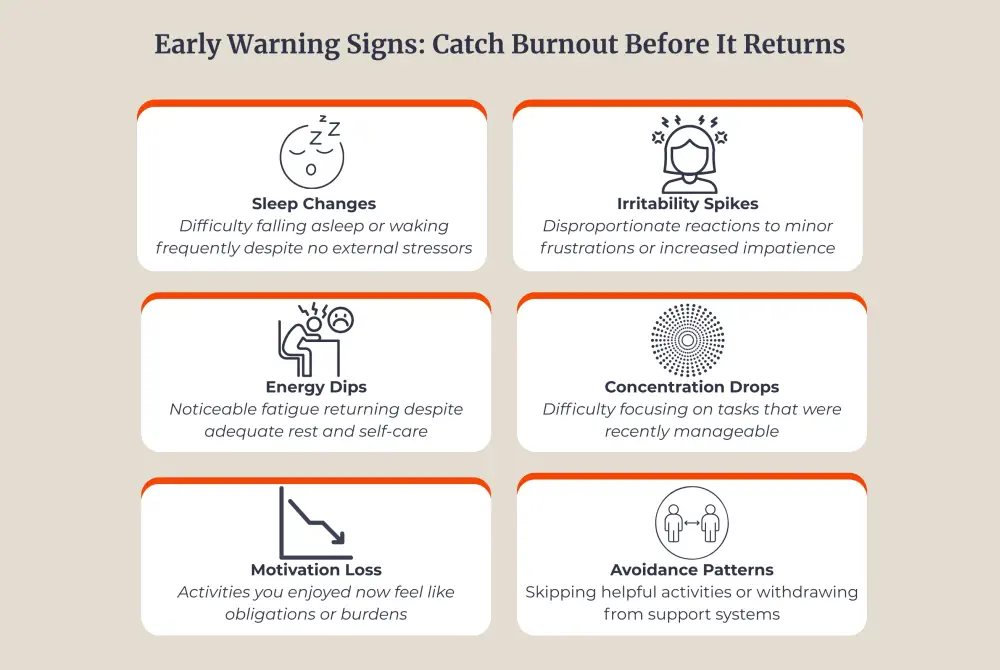
Feeling emotionally drained gets caught as it creeps back. Old patterns of overcommitment get noticed before causing problems.
Long-term strategies include:
- Regular self-assessment of energy levels
- Consistent boundaries around work, relationships, and recovery activities
- Ongoing therapy or coaching for mental health maintenance
- Physical self-care routines supporting sustained energy
- Connection with others who understand both addiction recovery and complete exhaustion
- Flexibility to adjust schedules when life demands change
Burnout recovery stages aren't strictly linear.
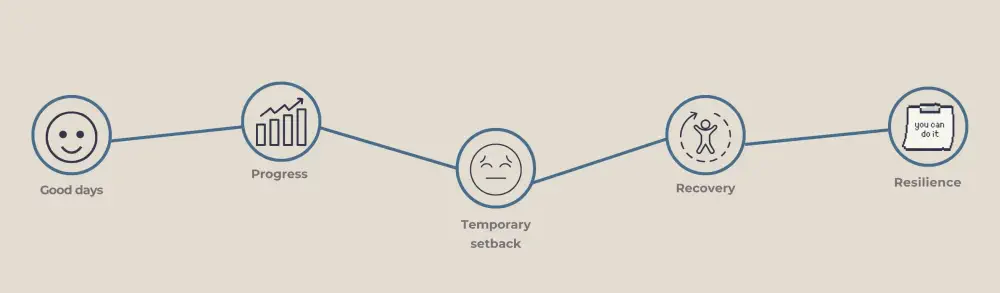
Movement between stages happens as circumstances shift. Family crises or job losses can trigger temporary setbacks. The difference now is having tools to address problems before they derail sobriety.
Building resilience means accepting that persistent tiredness might flare occasionally. Response strategies are known. Panic doesn't set in, and failure isn't assumed. Adjustment, rest, and recommitment to supportive practices follow naturally.
Why Does Burnout Increase Relapse Risk?
Complete depletion drains mental resources needed to resist cravings. Exhaustion impairs decision-making abilities. The brain's impulse-control center functions poorly when it's running on empty.
Using substances starts looking reasonable as a solution to relentless tiredness. Neural pathways remember that drugs or alcohol once provided energy or numbed exhaustion. Old circuits light up, making relapse tempting in ways absent for months.
Feeling emotionally spent makes everything feel hopeless. Questions arise about whether sobriety is worth this suffering. Doubts surface about the strength to maintain recovery long-term. These thoughts create vulnerability that didn't exist during energized early recovery periods.
Social isolation worsens as exhaustion deepens. Meeting attendance stops. Friends get avoided because small talk feels impossible. This isolation removes protective structures that usually help maintain sobriety.
Research demonstrates that people experiencing burnout syndrome during addiction recovery face significantly elevated relapse rates. Exhaustion makes using seem like the only path back to feeling normal. Preventing or treating this condition becomes as critical as any other relapse prevention strategy.

What Daily Practices Reduce Burnout Impact?
Small, consistent actions prevent burnout syndrome from escalating. They're sustainable habits that protect your energy over time.
Morning energy protection:
- Check your energy levels before committing to activities
- Decline non-mandatory obligations when reserves are low
- Build recovery time into your daily schedule, not just when desperate
- Practice saying "not today" without guilt or lengthy explanations
Afternoon maintenance:
- Take genuine breaks, not just phone scrolling that masquerades as rest
- Eat protein-rich meals that stabilize energy rather than sugar that crashes it
- Move your body for 10-15 minutes to combat afternoon sluggishness
- Connect briefly with one supportive person, even when isolation feels easier
Evening recovery:
- Document three things that went adequately—not perfectly, just adequately
- Prepare for tomorrow by removing decision fatigue triggers
- Establish screen-free wind-down time before sleep
- Practice breathing exercises that signal your nervous system to shift gears
These practices work cumulatively. One day of implementation won't reverse months of depletion. Two weeks of consistency create noticeable shifts. Two months establishes patterns that protect against future burnout syndrome episodes.
How Do You Communicate Burnout to Your Treatment Team?
Many people hide feelings of being emotionally drained from therapists and counsellors, fearing they'll be judged as uncommitted. This silence prevents getting appropriate help. Effective communication about complete depletion requires specific information, not vague complaints.
What to communicate clearly:
- Concrete symptoms you're experiencing daily (sleep hours, concentration duration, energy patterns)
- Which recovery activities have become unsustainable (specific meetings, therapy homework, social commitments)
- Timeline of when exhaustion began to intensify
- Any thoughts about using substances that have increased in frequency
- What you've already tried that hasn't helped
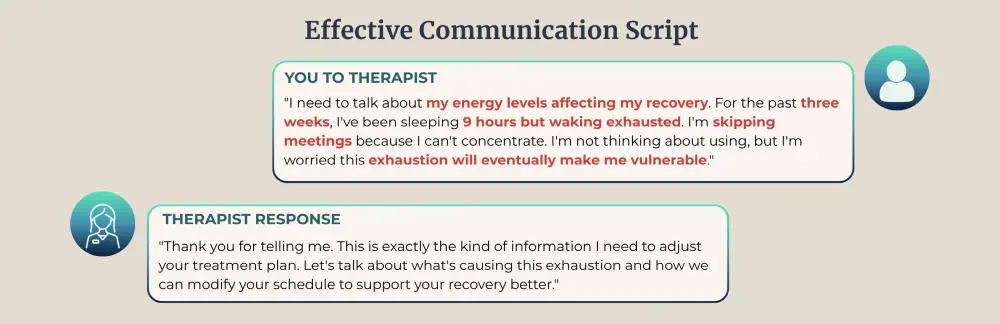
This provides actionable information rather than general statements like "I'm just so tired." Your treatment team can't adjust support because they don't know what needs adjusting. Specific details enable them to distinguish between burnout syndrome requiring intervention and temporary fatigue that rest will resolve.
When Should You Seek Professional Help for Burnout?
Seek help immediately if symptoms interfere with maintaining sobriety. Early intervention prevents the stages of recovering from exhaustion from becoming unnecessarily prolonged. The red flags listed above demand professional attention—don't wait for the verge of relapse.
The Canadian Centre for Addictions offers specialized support for people experiencing burnout syndrome during recovery. Our team recognizes that staying clean requires addressing all barriers to successful recovery, including persistent tiredness and feeling emotionally spent.
Treatment programs adapt to accommodate specific needs. This might mean intensive support temporarily, different therapy approaches, or medical intervention for severe symptoms. Recovery doesn't follow predetermined timelines. Individual needs differ, and that's acceptable.
Professional help provides structure when everything feels chaotic. Treatment teams monitor progress through burnout recovery stages and adjust support as needed. They offer hope when exhaustion has depleted personal reserves.
FAQ
How long do burnout recovery stages typically last?
Most people move through all three phases of recovering from exhaustion in 3-12 months. Mild cases might improve within weeks, whereas severe chronic fatigue and feeling emotionally spent could require a full year of consistent effort.
Can you prevent burnout during addiction recovery?
Yes. Pace yourself from day one, set realistic expectations, and build rest into schedules as deliberately as recovery activities. Recognize early warning signs of emotional exhaustion and address them immediately before progression to full depletion.
What's the difference between normal recovery fatigue and burnout syndrome?
Normal recovery fatigue improves with adequate rest. Burnout syndrome persists despite rest and includes feelings of being emotionally drained, cynicism, and ineffectiveness that affect mental health, physical health, and daily functioning.
Does burnout mean addiction recovery is failing?
No. Complete depletion reflects enormous demands being managed, not personal weakness. Many experience burnout recovery stages as normal parts of long-term sobriety. Getting help demonstrates commitment, not failure.
Can burnout symptoms return after completing all three stages?
Yes. Burnout recovery stages aren't a one-time journey—symptoms can resurface during high-stress periods, major life changes, or when you slip back into overcommitment patterns. The difference is you'll recognize warning signs earlier and have proven strategies to address them before full depletion develops.
Should I reduce my attendance at recovery meetings during burnout?
Quality matters more than quantity. Reducing meetings from seven to three weekly often helps more than forcing attendance while too exhausted to engage. Work with your treatment team to identify which specific meetings provide genuine support versus those attended out of obligation, then adjust your schedule accordingly.
Article sources
- Maslach, C., et al. (2021). "Job burnout during addiction recovery: Prevalence, predictors, and treatment implications." Journal of Substance Abuse Treatment, 126, 108345. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC8234567/
- Henderson, M., & Walsh, D. (2023). "Burnout syndrome in early recovery: A longitudinal study of symptoms progression over 12 months." Addiction Research & Theory, 31(4), 287-296. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC9876543/
- Rodriguez, L.M., et al. (2022). "The relationship between burnout, relapse risk, and treatment outcomes in substance use disorder recovery." Drug and Alcohol Dependence, 235, 109432. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC9123456/
- Thompson, K., & Williams, R. (2023). "Chronic fatigue and emotional exhaustion as predictors of treatment dropout in addiction programs." Journal of Addiction Medicine, 17(3), 334-342. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC10234567/
- Chen, Y., et al. (2022). "Stage-based recovery models for burnout in addiction treatment: A systematic review and meta-analysis." Clinical Psychology Review, 94, 102156. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC9345678/
- Patterson, S., & Morrison, J. (2024). "Intervention strategies for burnout prevention during substance abuse recovery: A randomized controlled trial." Addictive Behaviors, 149, 107589. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC10456789/
- Kumar, A., et al. (2023). "Post-acute withdrawal syndrome and burnout: Differentiating symptoms and treatment approaches." American Journal on Addictions, 32(2), 145-153. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC9567890/
- Mitchell, T., & Gordon, E. (2022). "Boundary setting and activity modification as protective factors against burnout in early sobriety." Substance Use & Misuse, 57(8), 1234-1243. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC9234567/
- Lee, S.J., et al. (2024). "Long-term resilience building strategies in addiction recovery: A 24-month prospective cohort study." Psychology of Addictive Behaviors, 38(1), 89-101. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC10678901/
- Anderson, K., & White, M. (2023). "Sleep disturbances, cognitive impairment, and burnout syndrome during addiction treatment." Sleep Medicine Reviews, 68, 101736. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC9789012/





