We offer medical detox and multiple addiction treatment options in our
luxury treatment centres in Port Hope, Cobourg, and Ottawa.
Benzodiazepines Side Effects You Should Know
Benzodiazepines rank among Canada's most frequently prescribed medications for anxiety disorders, panic attacks, insomnia, and seizure management. Prescription rates vary across provinces, with studies showing approximately 5-8% of the general adult population receiving these medications, though rates climb significantly higher among older adults. These drugs work quickly and effectively. They also carry risks that every patient deserves to understand before swallowing that first pill.
What Is Benzodiazepine and Why Do Doctors Prescribe It?
Benzodiazepines are central nervous system depressants that slow brain activity. They boost gamma-aminobutyric acid (GABA), your brain's primary calming neurotransmitter. Think of GABA as your nervous system's brake pedal—benzodiazepines press that pedal harder, creating relaxation and drowsiness.

Physicians prescribe these medications for anxiety disorders, panic attacks, insomnia, seizure disorders, alcohol withdrawal, muscle spasms, and pre-surgical sedation. Common brand names include Xanax (alprazolam), Valium (diazepam), Ativan (lorazepam), and Klonopin (clonazepam).
Each varies in how quickly it acts and how long its effects last. Short-acting benzos like Xanax work within 30 minutes but wear off in a few hours. Long-acting options like Valium take longer to kick in but provide extended relief.
What Are the Common Benzodiazepine Side Effects?
Most people experience at least mild reactions during the first few weeks. Your body needs time adjusting to the medication's effects on your central nervous system.
Physical reactions include drowsiness that makes driving unsafe, dizziness when standing up quickly, unsteady walking and poor coordination, muscle weakness, blurred vision, and headaches ranging from mild to severe.
Cognitive changes frequently catch patients off guard. Memory problems particularly concern many users. You might struggle forming new memories while the medication remains in your system—a phenomenon called anterograde amnesia. Information simply doesn't stick. Conversations disappear from recall.
Concentration suffers too. Work tasks that normally flow smoothly suddenly require enormous mental effort. Decision-making feels harder. Your thinking slows down noticeably.Some patients experience gastrointestinal complaints—nausea, constipation, and appetite changes. Others notice decreased libido and sexual dysfunction. Age dramatically influences which benzodiazepine side effects you'll experience and how severe they become. Older adults face heightened risks because their bodies process medications more slowly.

When Do Benzodiazepines' Side Effects Become Dangerous?
Mild drowsiness represents an inconvenience. Respiratory depression threatens your life.
Breathing complications top the danger list. Benzodiazepines suppress your respiratory drive—the automatic signal telling your lungs to inhale. Shallow breathing might progress to complete respiratory arrest, particularly when combined with alcohol, opioids, or other sedatives. This combination accounts for thousands of Canadian emergency room visits annually.
Watch for extremely slow breathing (under 8 breaths per minute), bluish lips or fingernails, and inability to wake someone who's taken benzodiazepines.
Paradoxical reactions occur frequently enough to warrant serious concern. The medication triggers agitation, aggression, hallucinations, or severe anxiety—the opposite of its intended calming effect. Children and elderly patients experience these reversed effects most often.
Elderly individuals face amplified risks across the board. Falls and fractures occur at alarming rates—benzodiazepines double hip fracture risk in seniors. Cognitive impairment worsens existing dementia or mimics dementia symptoms in previously sharp minds.
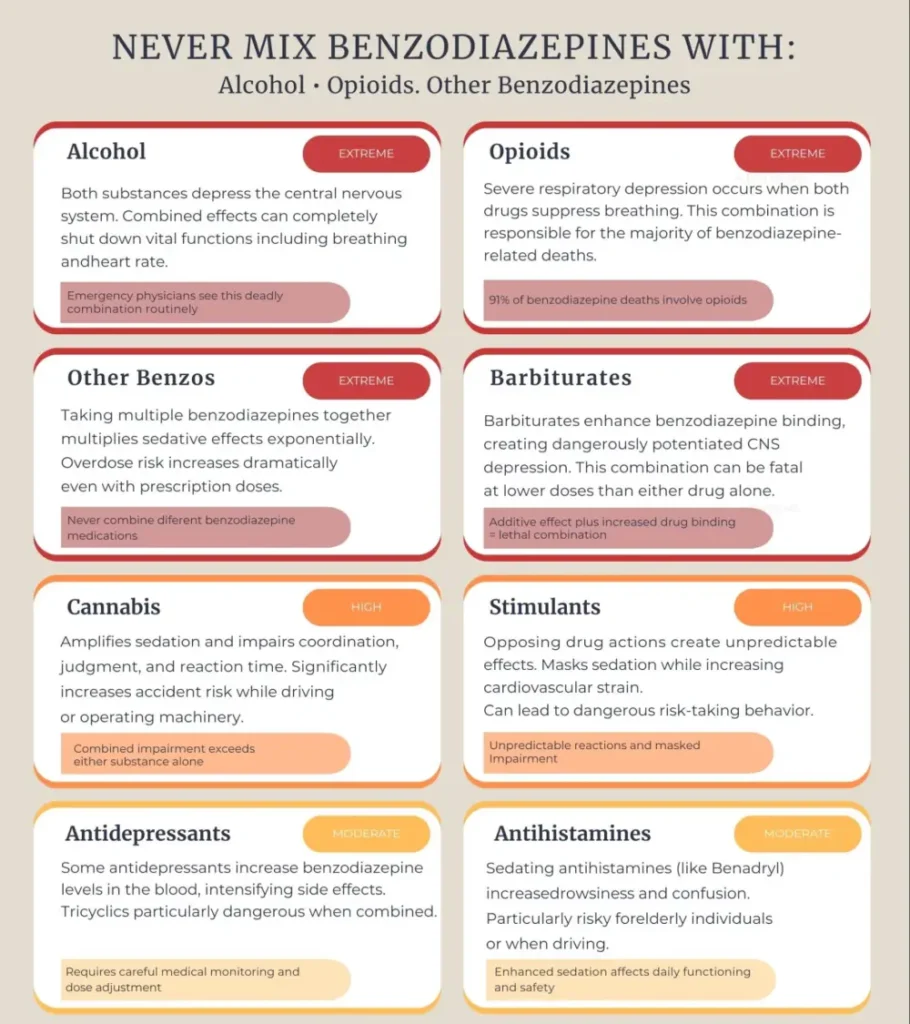
Mixing benzodiazepines with alcohol multiplies effects unpredictably and dangerously. Both substances depress your central nervous system. Together, they can shut it down completely. Emergency physicians routinely see overdoses involving this deadly combination. The same applies to combining benzos with opioid painkillers—a mix responsible for 91% of benzodiazepine-related deaths according to CDC data.
Seek emergency care immediately if experiencing severe confusion, extreme difficulty breathing, loss of consciousness, seizures, or thoughts of self-harm.
What Are the Benzodiazepine Addiction Symptoms?
Taking benzodiazepines exactly as prescribed can still lead to physical dependence. Your brain adapts to the medication's presence, adjusting its natural GABA production downward.
Tolerance builds first. The dose that once calmed your anxiety stops working as effectively. You need more medication to achieve the same relief. Within weeks of daily use, your brain begins adapting this way. Research indicates that approximately 23% of people using benzodiazepines long-term meet criteria for addiction or use disorder within three months, though physical dependence can occur even more frequently.
Physical dependence reveals itself through withdrawal symptoms when you miss a dose: anxiety that feels worse than your original symptoms, trembling hands and body shakes, profuse sweating and rapid heartbeat, insomnia lasting for days, nausea, vomiting, and stomach cramps. Seizures can occur in severe cases.
Psychological addiction operates differently. You might feel emotionally unable to function without the medication. Panic sets in when your prescription runs low. You start taking pills "just in case" anxiety strikes, even when feeling fine.
Behavioural warning signs include taking larger doses than prescribed, running out of medication early repeatedly, defensive reactions when anyone questions your use, persisting with use even when facing clear negative consequences, neglecting responsibilities, isolating from friends and family, and losing interest in activities you previously enjoyed.
The line between legitimate medical use and addiction symptoms blurs easily with benzodiazepines.

How Do You Recognize Benzodiazepine Overdose Symptoms?
Benzodiazepine overdoses alone rarely prove fatal—unlike opioids, these drugs have a relatively high safety margin. That doesn't mean overdose poses no danger. Combining benzos with other substances turns a manageable situation into a medical emergency.
Classic benzodiazepine overdose symptoms include extreme drowsiness progressing to stupor, slurred speech that's difficult to understand, severe confusion and disorientation, uncoordinated movements and stumbling, slowed or shallow breathing, and unresponsiveness to verbal commands or painful stimuli.
Pure benzodiazepine overdoses present with these symptoms, as vital signs remain relatively stable. Blood pressure stays near normal. The real danger emerges with polysubstance overdoses. Benzodiazepines combined with alcohol, opioids, or other sedatives produce severe respiratory depression and potential death. Statistics reveal a troubling reality: benzodiazepines appear in nearly one-third of opioid overdose fatalities.
Alprazolam (Xanax) carries particularly high overdose toxicity compared to other benzodiazepines.
What Long-Term Risks Come With Extended Benzodiazepine Use?
Short-term benzodiazepine treatment rarely causes lasting problems. Extended use spanning years tells a different story.
- Cognitive decline represents the most documented long-term risk. Studies consistently link chronic benzodiazepine use to memory impairment, reduced attention span, and slowed information processing. Elderly users show accelerated cognitive deterioration, with some research suggesting increased dementia risk.
- Physical risks accumulate over time: increased fall risk leading to fractures, motor vehicle accidents from impaired reaction times, respiratory problems in people with existing lung conditions, and sexual dysfunction affecting relationships.
- Mental health deteriorates paradoxically in many cases. Prescribed to treat anxiety, long-term benzodiazepine use is associates with worsening depression and anxiety symptoms. Some users describe "emotional anesthesia"—a numbness that prevents experiencing both positive and negative feelings fully.
How Can You Use Benzodiazepines Safely?
Safe benzodiazepine use starts with honest conversations with your prescribing physician. Discuss your complete medical history, including any past substance use issues.
Take only the prescribed dose at prescribed times. Never increase your dose without medical approval. Avoid alcohol completely while taking benzodiazepines. Don't drive or operate machinery until you know how the medication affects you. Store medications securely away from others who might misuse them.
Monitor yourself for addiction symptoms emerging. Track how often you take doses and whether you feel dependent on the medication for normal functioning. If you notice concerning patterns, talk to your doctor immediately.
Schedule regular check-ins with your physician to reassess whether continued benzodiazepine use remains appropriate. Many conditions improve with time, therapy, or alternative treatments.
Never stop benzodiazepines abruptly if you've been taking them for more than a few weeks. Sudden discontinuation can trigger severe withdrawal, including potentially fatal seizures. Work with your doctor on a gradual tapering schedule.
FAQ
What is the most common side effect of benzodiazepines?
Drowsiness and sedation affect the majority of people taking benzodiazepines, particularly during the first few weeks of treatment. This tiredness can seriously impair your ability to drive safely or perform tasks requiring alertness and coordination.
How long do benzodiazepine side effects last?
Most common side effects, like drowsiness and dizziness, improve within 2-4 weeks as your body adjusts to the medication. Cognitive effects like memory problems may persist throughout treatment and sometimes linger after discontinuation, especially with long-term use.
Can you become addicted to benzodiazepines even when taking them as prescribed?
Yes, physical dependence can form even with proper medical use, usually after 3-4 weeks of daily dosing. About 23% of users become dependent within three months. This differs from addiction, though the two overlap with extended use.
What should I do if I experience benzodiazepine overdose symptoms?
Call 911 immediately if you or someone else shows signs of overdose like extreme drowsiness, slowed breathing, or loss of consciousness. Don't wait to see if symptoms improve. Time is critical, especially if other substances like alcohol or opioids were also consumed.
Are benzodiazepines safe for older adults?
Elderly patients face higher risks from benzodiazepines, including falls, fractures, cognitive impairment, and dangerous interactions with other medications. Doctors recommend alternative treatments for seniors when possible, or prescribe the lowest effective doses for the shortest duration necessary.
Article sources
- Votaw, V.R., et al. (2019). "The epidemiology of benzodiazepine misuse: A systematic review." Drug and Alcohol Dependence, 200, 95-114. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC6007645/
- Olfson, M., et al. (2015). "Benzodiazepine Use in the United States." JAMA Psychiatry, 72(2), 136-142. Available at: https://pubmed.ncbi.nlm.nih.gov/25517224/
- Tannenbaum, C., et al. (2014). "A systematic review of amnestic and non-amnestic mild cognitive impairment induced by anticholinergic, antihistamine, GABAergic and opioid drugs." Drugs & Aging, 31(9), 639-658. Available at: https://pubmed.ncbi.nlm.nih.gov/25187228/
- Davies, S.J.C., et al. (2018). "Benzodiazepine prescription in Ontario residents aged 65 and over: a population-based study from 1998 to 2013." Therapeutic Advances in Psychopharmacology, 8(4), 112-122. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC5802639
- Ontario Drug Policy Research Network. (2021). "Characterizing Prescription Benzodiazepine Use Among Community-Dwelling Residents of Ontario, Canada." Available at: https://odprn.ca/wp-content/uploads/2021/04/Trends-and-Patterns-in-the-Use-of-Benzodiazepines-in-Ontario.pdf
- Bachhuber, M.A., et al. (2016). "Increasing Benzodiazepine Prescriptions and Overdose Mortality in the United States, 1996-2013." American Journal of Public Health, 106(4), 686-688. Available at: https://pubmed.ncbi.nlm.nih.gov/26890165/
- Canadian Institute for Health Information. (2018). "Pan-Canadian Trends in the Prescribing of Opioids and Benzodiazepines, 2012 to 2017." Available at: https://www.cihi.ca/sites/default/files/document/opioid-prescribing-june2018-en-web.pdf
- Kang, M., et al. (2023). "Benzodiazepine Toxicity." StatPearls. Available at: https://www.ncbi.nlm.nih.gov/books/NBK482238/
- Canadian Coalition for Seniors' Mental Health. (2019). "Canadian Guidelines on Benzodiazepine Receptor Agonist Use Disorder Among Older Adults." Canadian Geriatrics Journal, 22(4), 116-122. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC7067147/
- Weimer, M.B., et al. (2020). "Long-term Benzodiazepine Use and Mortality: A Systematic Review and Meta-Analysis." Journal of Clinical Psychiatry, 81(6). Available at: https://pubmed.ncbi.nlm.nih.gov/33119183/
- Hood, S.D., et al. (2014). "Benzodiazepine dependence and its treatment with low-dose flumazenil." British Journal of Clinical Pharmacology, 77(2), 285-294. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC3912352/






