We offer medical detox and multiple addiction treatment options in our
luxury treatment centres in Port Hope, Cobourg, and Ottawa.
Alcohol Withdrawal Timeline: First Weeks
Stopping alcohol after years of heavy drinking triggers a cascade of physical and mental reactions. Your body has adapted to constant alcohol presence. Now it must relearn how to function without it.
The alcohol withdrawal symptoms timeline varies dramatically between individuals. Some people breeze through with minor discomfort. Others face life-threatening complications requiring immediate medical intervention.

Key takeaway:
- How your first 6-12 hours unfold and why hand tremors, sweating, and anxiety aren't just a bad hangover—they signal your central nervous system scrambling to function without alcohol's depressant effects
- When symptoms intensify between 12-24 hours, and what hallucinations (seeing shadows, hearing voices) actually mean about your brain's GABA receptors suddenly receiving zero input while glutamate goes into overdrive
- Why the 24-48 hour window proves most dangerous and which specific warning signs (muscle twitching, jaw clenching, blood pressure spikes) predict seizures before they strike—even in people with no epilepsy history
- What delirium tremens looks like during hours 48-72, and why only 3-5% experience it, yet 15-37% of those cases turn fatal without medical intervention
- How long acute symptoms persist beyond 72 hours, and why psychological challenges (anxiety, depression, anhedonia) can extend for months through post-acute withdrawal syndrome
- Which personal factors determine your severity, including how daily vodka drinkers face 40-60% GABA receptor downregulation versus 15-20% for occasional beer drinkers, and why this matters desperately
- Why previous withdrawal attempts worsen each subsequent detox through the kindling effect that permanently increases glutamate receptors per cycle, raising seizure risk
When Do Alcohol Withdrawal Symptoms Begin Hour by Hour?
Physical reactions typically begin within 6-12 hours after your last drink, though some people don't notice changes for up to 24 hours. Your body starts protesting the absence of alcohol almost immediately, even while you sleep.

First 6-12 Hours: What Are the Initial Warning Signs?
Tremors start in your hands. You might wake up sweating despite cool temperatures.
Your head aches. Nausea creeps in, sometimes accompanied by vomiting. Anxiety ratchets up even though nothing particularly stressful is happening. Sleep becomes impossible even when you're exhausted.
These early reactions reflect your central nervous system suddenly working without alcohol's depressant effects. Your brain chemistry scrambles to compensate. Neurotransmitters fire erratically because they've grown accustomed to chronic alcohol use moderating their activity.
People often confuse these signs with a bad hangover. The distinction matters—hangovers resolve within hours, but these reactions intensify.
12-24 Hours: Why Do Symptoms Intensify?
Everything from the first phase amplifies. Hand tremors spread to your arms and legs. Sweating drenches your clothes.
Some individuals experience visual or auditory hallucinations during this window. You might see shadows moving at the edge of your vision. Sounds become distorted, or you hear voices that aren't there. These hallucinations usually signal severe reactions requiring immediate medical attention.
Your heart races. Blood pressure climbs. Confusion clouds your thinking even for simple decisions.
Brain chemistry changes drive this escalation. GABA receptors, which alcohol normally activates to calm neural activity, suddenly receive no input. Meanwhile, glutamate receptors go into overdrive, creating a hyperactive nervous system state.
24-48 Hours: What Makes This Window Most Dangerous?
Seizure risk peaks during these hours. Grand mal seizures can strike people with no epilepsy history.
Medical supervision becomes critical now. Healthcare providers watch for muscle twitching, jaw clenching, and rising blood pressure—early seizure indicators that allow preventive medication administration before full convulsions occur.
Hallucinations intensify for those experiencing them. Disorientation increases. Some people become agitated or aggressive due to confusion about their surroundings.
48-72 Hours: When Do Symptoms Reach Their Peak?
Delirium tremens (DTs) can emerge during this timeframe for high-risk individuals. Only 3-5% of people experience DTs, but the condition proves fatal in 15-37% of cases without medical treatment. Modern intensive care reduces mortality to 1-5%.
DTs manifestations include:
- Severe confusion and disorientation
- Vivid hallucinations (visual, auditory, tactile)
- Profound agitation or paranoia
- Fever exceeding 101°F (38.3°C)
- Racing heart rate above 100 beats per minute
- Dangerously high blood pressure
- Profuse sweating
This represents a medical emergency requiring immediate hospitalization. Detox from alcohol in a supervised setting prevents DTs through appropriate medication protocols.
Most people without DTs see their reactions peak during these hours, then gradually decline. Physical discomfort begins easing. The worst passes, though challenges continue.
Beyond 72 Hours: How Long Until Symptoms Improve?
Physical reactions steadily diminish after the 72-hour mark. Tremors fade. Nausea subsides. Sleep patterns slowly normalize, though quality rest may take weeks to return fully.
Psychological challenges prove more persistent. Anxiety lingers for weeks. Depression can emerge or worsen, particularly if you were drinking to self-medicate mood disorders. Irritability tests your patience and strains relationships.
Some people experience post-acute withdrawal syndrome (PAWS)—reactions continuing for months after the acute phase ends. PAWS manifestations include:
- Mood swings without clear triggers
- Difficulty concentrating
- Sleep disturbances despite physical recovery
- Anhedonia (inability to feel pleasure)
- Memory problems
- Ongoing anxiety
The extended alcohol detox timeline prepares you for recovery's true duration. Alcohol addiction treatment addresses these prolonged challenges through therapy, medication management, and coping skills development.
What Factors Determine Your Personal Withdrawal Timeline?
Multiple variables influence severity and duration through specific biological mechanisms. Two people with similar drinking patterns can have vastly different reactions due to these underlying physiological differences.
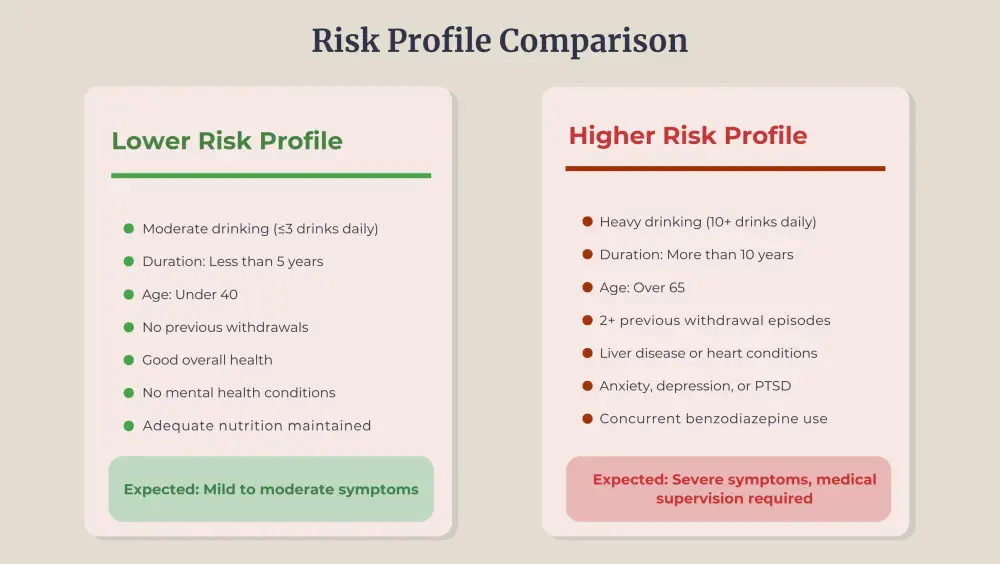
Does the Amount You Drink Change Withdrawal Severity?
Alcohol consumption patterns alter your brain's receptor density. Heavy daily drinking for years causes substantial GABA receptor downregulation—your brain produces fewer receptors because alcohol constantly activates them. When you stop, the shortage leaves you with inadequate natural calming mechanisms.
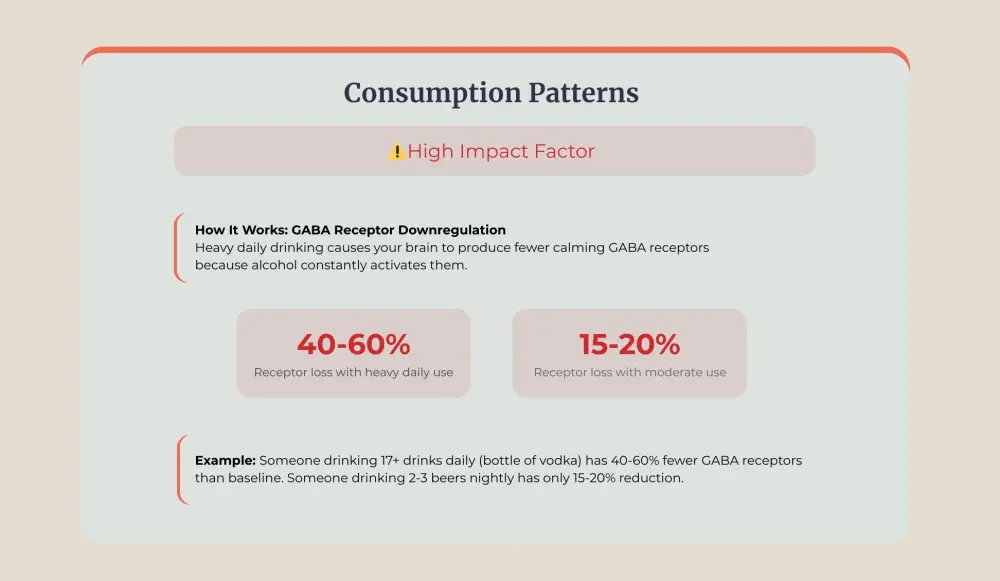
Binge drinking patterns create different neural adaptations. Intermittent heavy use prevents stable receptor equilibrium, causing erratic neurological responses during cessation. Your brain never fully adapts to either drinking or sobriety.
How Do Age and Overall Health Affect Withdrawal?
Liver enzyme activity determines how quickly your body clears alcohol and its toxic metabolites. The CYP2E1 enzyme, responsible for alcohol metabolism, declines approximately 0.5% annually after age 40. By age 65, enzyme activity drops 12-15%, extending detoxification by days.
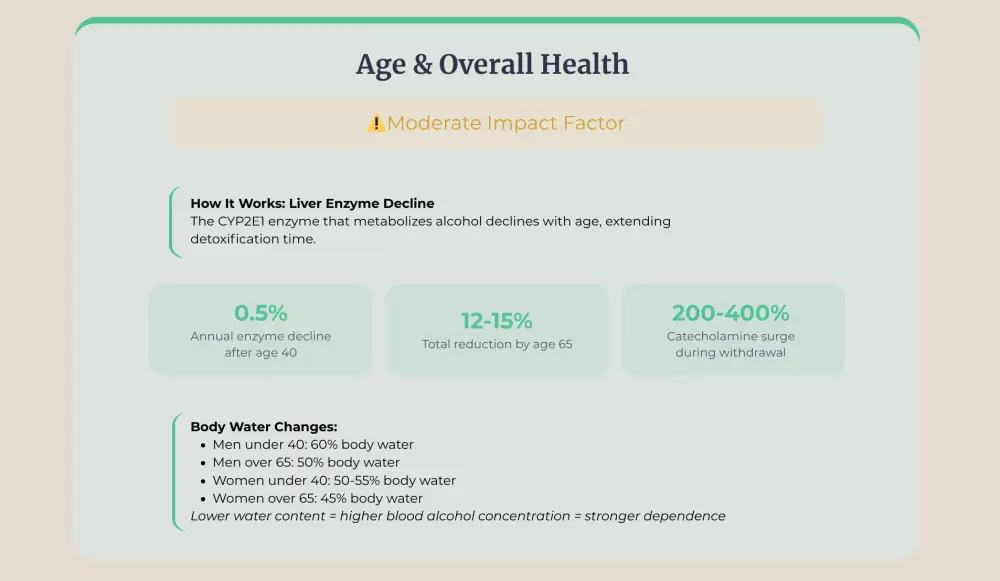
Cardiovascular conditions compound withdrawal dangers through specific mechanisms. Sympathetic nervous system activation during cessation increases norepinephrine and epinephrine by 200-400%. Pre-existing heart disease cannot handle this sudden catecholamine surge, triggering arrhythmias or myocardial infarction.
Why Do Previous Withdrawals Make It Worse?
The kindling effect operates through progressive NMDA receptor sensitization. Each withdrawal cycle increases glutamate receptor density by 15-25%. More receptors mean more excitatory signalling during subsequent cessations.
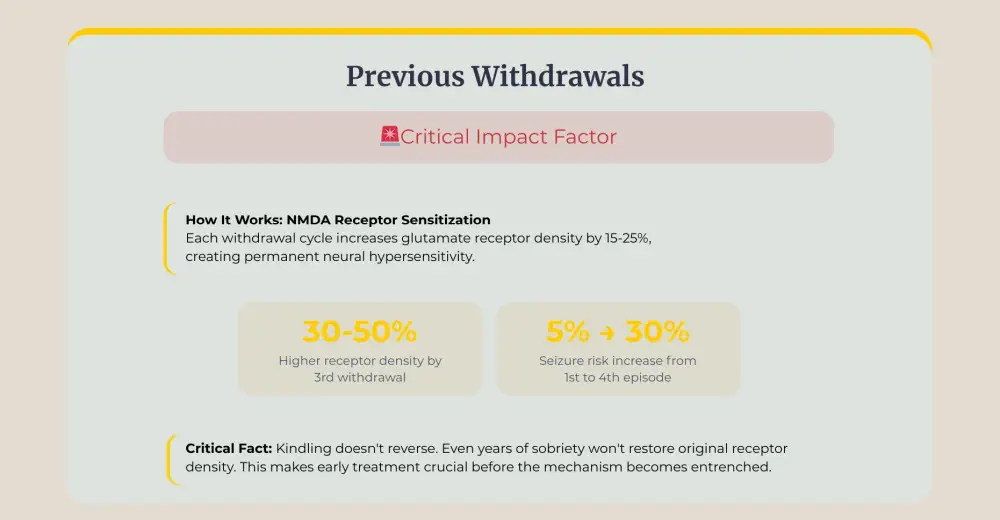
Your brain keeps these altered receptor patterns indefinitely. Maintaining sobriety for years, even decades, cannot undo the neurological changes that withdrawal cycles create. Getting help before multiple detox episodes occur prevents the brain from locking in this heightened sensitivity. Early intervention stops the damage while it can still be limited.
What Role Do Co-Occurring Conditions Play?
Mental health disorders share neurological pathways with alcohol dependence, creating compounding effects during cessation. Anxiety disorders involve dysregulated GABA transmission, the same system that alcohol disrupts. Removing alcohol while GABA receptors are already compromised triggers severe panic responses and potentially dangerous blood pressure spikes.
Polysubstance use complicates withdrawal through receptor cross-tolerance. Benzodiazepines and alcohol both activate GABA receptors. Simultaneous dependence creates 70-90% receptor downregulation compared to 40-60% with alcohol alone. Cessation reactions amplify proportionally.
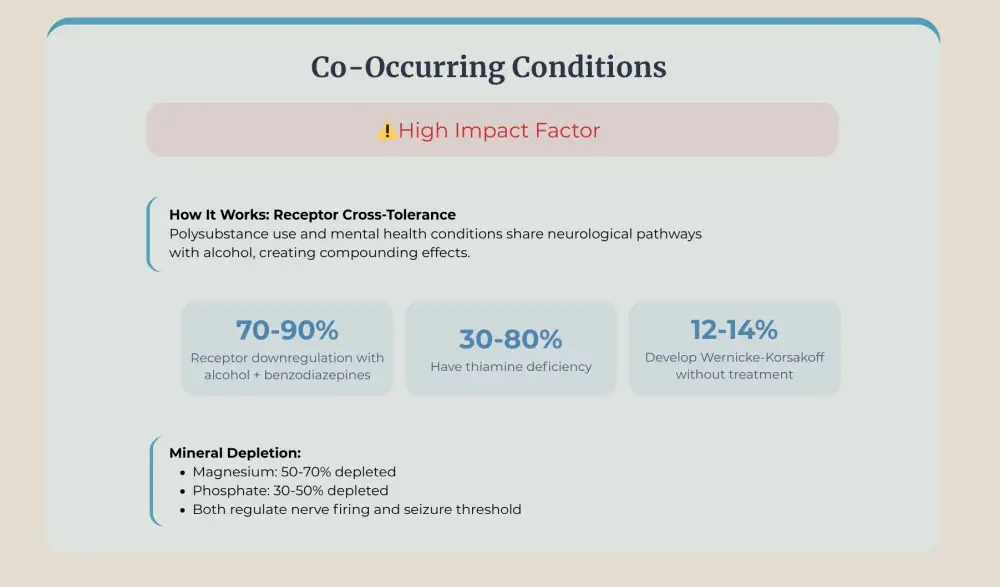
Thiamine deficiency, present in 30-80% of people with chronic alcohol use, disrupts glucose metabolism in brain cells. During withdrawal's metabolic stress, thiamine-depleted neurons cannot produce adequate energy. This triggers Wernicke-Korsakoff syndrome: confusion, vision problems, and permanent memory damage affecting 12-14% of untreated detox patients.
Electrolyte imbalances create additional neurological stress. Chronic drinking depletes magnesium by 50-70% and phosphate by 30-50%. These minerals regulate nerve firing. Deficiency during withdrawal lowers the seizure threshold substantially.
Why Is Medical Supervision Critical During Alcohol Detox?
Alcohol cessation can kill you through multiple mechanisms that medical monitoring prevents. Professional care reduces mortality from 15-37% to under 5% through early intervention protocols.
What Medical Monitoring Actually Involves
Nurses assess you using the CIWA-Ar (Clinical Institute Withdrawal Assessment for Alcohol) scale every 2-4 hours. This 10-item questionnaire scores:
- Nausea/vomiting (0-7 points)
- Tremor intensity (0-7 points)
- Sweating severity (0-7 points)
- Anxiety level (0-7 points)
- Agitation (0-7 points)
- Tactile/auditory/visual disturbances (0-7 points each)
- Headache (0-7 points)
- Orientation/clouding of sensorium (0-4 points)
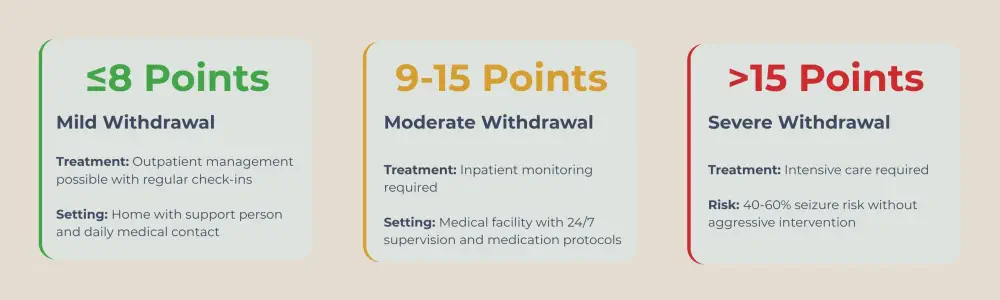
Vital signs get checked every 2-4 hours: heart rate, blood pressure, temperature, respiratory rate, oxygen saturation. Sudden spikes—blood pressure jumping from 120/80 to 180/110 within an hour—indicate imminent seizures requiring immediate benzodiazepine administration.
Blood work monitors electrolytes (sodium, potassium, magnesium, phosphate), liver function (AST, ALT, bilirubin), and thiamine levels. Abnormalities get corrected intravenously before they trigger complications.
How Medications Prevent Complications
Benzodiazepines work by enhancing GABA receptor activity, temporarily compensating for alcohol's absence. Diazepam (Valium) provides the longest action—single doses continue working 20-100 hours, maintaining steady nervous system suppression.
Dosing follows symptom-triggered protocols: CIWA-Ar scores of 8-15 trigger 10-20mg diazepam. Scores above 15 require 20mg doses repeated until symptoms subside. Some patients need 200-400mg daily during peak withdrawal—massive doses are tolerable only under medical supervision.
Anti-seizure medications like carbamazepine block sodium channels in neurons, preventing the electrical storms that cause convulsions. Gabapentin enhances GABA transmission through different receptors than benzodiazepines, providing additional seizure protection plus craving reduction.
Thiamine 500mg intravenously daily prevents Wernicke's encephalopathy. Oral thiamine is poorly absorbed—only 5-10% reaches the bloodstream. IV administration delivers 100% directly to tissues, protecting the brain during metabolic stress.
Beta-blockers like propranolol control the catecholamine surge that drives dangerous increases in heart rate and blood pressure. They reduce cardiac workload by 30-40%, preventing arrhythmias and heart attacks in vulnerable patients.
Detox Environment
Quiet, dimly lit rooms reduce sensory overstimulation that worsens confusion and agitation. Bright lights and loud noises amplify glutamate excitatory signals already overwhelming your nervous system.
Frequent reorientation (staff regularly reminding you of the date, location, and situation) combats the confusion component of withdrawal delirium. Physical calendars, clocks, and windows help anchor you to reality when your brain struggles with basic awareness.
Staff-to-patient ratios of 1:2 or 1:3 allow continuous observation. DTs can escalate from mild confusion to life-threatening cardiovascular collapse within 30-60 minutes. Close monitoring catches deterioration early.
What Happens After Detox Stabilizes
Supervised alcohol detox lasts 5-10 days for most people. Your body clears alcohol and acute withdrawal resolves. But alcohol withdrawal symptoms represent only the beginning.
Psychological dependence remains intact. Therapy explores why you drank, identifies triggers, and builds coping skills. Individual counselling addresses personal trauma and mental health conditions. Group therapy provides peer support and accountability.Long-term recovery demands sustained effort. Aftercare programs, support groups, and ongoing therapy help prevent relapse. Medical detox saves your life. Comprehensive treatment teaches you how to live it.

Get Professional Support for Safe Alcohol Detox
The Canadian Centre for Addictions provides medically supervised alcohol detox at our Ontario facilities. Our experienced healthcare team monitors you around the clock using CIWA-Ar protocols, manages reactions with appropriate medications, and ensures your safety throughout detoxification.
We recognize that facing cessation feels overwhelming. Our compassionate staff supports you through every difficult moment while connecting you with comprehensive treatment addressing the underlying alcohol addiction driving your drinking.
Don't risk your life attempting detox alone. Call us today at 1-855-499-9446 to learn about our medical detox programs and begin your recovery safely.
FAQ
What should I bring to medical detox?
Pack comfortable, loose clothing (withdrawal can cause temperature fluctuations), personal toiletries, any prescription medications with pharmacy labels, insurance cards, and contact information for a family member or support person. Most facilities initially prohibit electronics but later allow them. Don't bring valuables.
Can I continue working during outpatient detox?
No. Cognitive impairment, unpredictable symptom severity, and seizure risks make working unsafe for you and others. Even mild withdrawal affects concentration, reaction time, and decision-making. Employers often accommodate medical leave for detox treatment.
How do I assess my personal seizure risk?
High-risk indicators include: previous withdrawal seizures, drinking 10+ drinks daily for years, history of head trauma, concurrent benzodiazepine use, previous DTs, age over 65, or underlying seizure disorders. Anyone with 2+ risk factors should never attempt home detox.
What's the difference between medical detox and rehab?
Medical detox manages acute physical withdrawal (5-10 days). Rehab addresses psychological addiction through therapy, education, and skill-building (30-90 days). Detox stabilizes your body. Rehab changes your relationship with alcohol. Both are typically needed for lasting recovery.
What if I can't afford medical detox?
Ontario hospitals provide emergency detox through provincial health coverage. Community health centres offer sliding-scale programs. The Canadian Centre for Addictions accepts most insurance plans and discusses payment options during confidential consultations. Never let cost prevent seeking medical care for potentially fatal withdrawal.
Should family members visit during detox?
Facilities vary. Some limit early visits because emotional interactions can worsen agitation during acute withdrawal. Others encourage family presence for reassurance. Ask admissions staff about policies. Phone calls may be restricted initially for similar reasons. Family participation typically increases after stabilization (day 3-5).
Article sources
- Sullivan, J.T., et al. (1989). "Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar)." British Journal of Addiction, 84(11), 1353-1357. Available at: https://pubmed.ncbi.nlm.nih.gov/2597811/
- Schuckit, M.A. (2014). "Recognition and management of withdrawal delirium (delirium tremens)." New England Journal of Medicine, 371(22), 2109-2113. Available at: https://www.nejm.org/doi/full/10.1056/NEJMra1407298
- Long, D., et al. (2017). "Alcohol withdrawal syndrome: Mechanisms, manifestations, and management." Neurology and Rehabilitation Journal, Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC5513695/
- Perry, E.C. (2014). "Inpatient management of acute alcohol withdrawal syndrome." CNS Drugs, 28(5), 401-410. Available at: https://pubmed.ncbi.nlm.nih.gov/24781751/
- Mayo-Smith, M.F. (1997). "Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline." JAMA, 278(2), 144-151. Available at: https://pubmed.ncbi.nlm.nih.gov/9214529/
- Sarai, S.K., et al. (2022). "Delirium tremens (DTs)." StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available at: https://www.ncbi.nlm.nih.gov/books/NBK482134/
- Thomson, A.D., et al. (2012). "The evolution and treatment of Korsakoff's syndrome: out of sight, out of mind?" Neuropsychology Review, 22(2), 81-92. Available at: https://pubmed.ncbi.nlm.nih.gov/22569770/
- Day, E., et al. (2013). "Thiamine for prevention and treatment of Wernicke-Korsakoff Syndrome in people who abuse alcohol." Cochrane Database of Systematic Reviews, (7), CD004033. Available at: https://pubmed.ncbi.nlm.nih.gov/23818101/
- Sachdeva, A., et al. (2015). "Alcohol withdrawal syndrome: Benzodiazepines and beyond." Journal of Clinical and Diagnostic Research, 9(9), VE01-VE07. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC4606320/
- Mirijello, A., et al. (2015). "Identification and management of alcohol withdrawal syndrome." Drugs, 75(4), 353-365. Available at: https://pubmed.ncbi.nlm.nih.gov/25666543/





