We offer medical detox and multiple addiction treatment options in our
luxury treatment centres in Port Hope, Cobourg, and Ottawa.
What Is the Difference Between CBT and DBT?
In 2017, it was estimated that 20.7 million Americans needed treatment for substance use disorders. Addiction recovery requires an approach uniquely tailored to each individual, so no two recoveries will be the same. Often, recovery will utilize a combination of individual therapy sessions and group programs. Understanding the root causes, instigators, and symptoms is key to long-term sustained recovery. This allows the individual in recovery to address the root issue rather than trying to escape their problem by using drugs or alcohol. While several different approaches may be used throughout recovery, two of the most common are Cognitive Behavioural Therapy (CBT) and Dialectical Behavioural Therapy (DBT).
Cognitive Behavioural Therapy (CBT) is a short-term, goal-oriented approach where the strategy is to change the pattern of thinking, thereby changing the way an individual feels. This hopefully results in changes to the individual’s behaviour. Dialectical Behavioural Therapy (DBT) is a form of CBT that addresses the emotional response to stimulation.
Key Takeaway:
- CBT Approach: Targets negative thought patterns through logical restructuring; typically 12-16 weeks of structured, goal-oriented treatment with homework assignments
- DBT Approach: Focuses on emotional regulation through acceptance and mindfulness; requires a 6-12 month commitment with both individual and group sessions
- Core Distinction: CBT asks, "Is this thought accurate?" while DBT asks, "How can I manage this emotion without destructive behaviour?"
- Treatment Match Matters: Depression, anxiety, and OCD respond better to CBT; borderline personality disorder, self-harm, and chronic suicidal ideation respond better to DBT
- Addiction Applications: CBT identifies triggers and faulty beliefs about substances; DBT addresses the emotional dysregulation that drives substance use
- Personal Fit: Your specific challenges, treatment goals, and how you respond to logical versus acceptance-based approaches determine which therapy works best
What Is Cognitive Behavioural Therapy?
Cognitive behavioural therapy operates on a straightforward premise: your thoughts directly influence your feelings and behaviours. Negative thought patterns create emotional distress, which then drives problematic actions. Change the thought, change the outcome.

Aaron Beck developed CBT in the 1960s after observing that depressed patients shared similar patterns of negative automatic thoughts. He noticed people telling themselves things like "I'm worthless" or "Nothing ever works out for me." These weren't random complaints. They were deeply ingrained cognitive distortions that shaped every interaction with the world.
CBT targets specific problems with measurable goals. Your therapist won't spend months exploring childhood memories. Instead, you'll identify exactly which thoughts cause trouble and develop concrete strategies to counter them.
Treatment typically runs 12 to 16 weeks. Sessions last about 45 to 60 minutes and happen weekly. Between appointments, you'll complete homework assignments that reinforce what you've learned. This structured approach makes progress trackable and keeps treatment focused.
Think of CBT as detective work. You examine evidence for and against your negative beliefs. When someone with social anxiety thinks "Everyone judges me harshly," CBT asks: What proof exists for this belief? What evidence contradicts it? Often, the evidence against negative thoughts far outweighs the evidence supporting them.
Core Techniques in CBT
Several techniques make cognitive behavioural therapy effective:
- Cognitive restructuring identifies distorted thinking patterns. Catastrophizing. Black-and-white thinking. Mind reading. Once you spot these patterns, you can challenge them before they spiral into emotional distress.
- Behavioural experiments test negative predictions in real-world situations. Believing a party will end in humiliation? You attend one and observe what actually happens. Reality often proves far less threatening than imagination suggests.
- Problem-solving skills break overwhelming challenges into manageable steps. Instead of feeling paralyzed by a mountain of debt, you create a realistic payment plan and tackle it systematically.
- Exposure therapy gradually confronts fears in controlled settings. Someone with a phobia of driving might start by sitting in a parked car, then progress to short trips around the block, eventually building up to highway driving.
CBT's logical framework appeals to people who respond well to reasoning and prefer concrete strategies over abstract exploration. You leave each session with actual tools to use throughout your week.
What Is Dialectical Behavioural Therapy?
Dialectical behavioural therapy emerged from a crisis. In the late 1980s, psychologist Marsha Linehan struggled to treat patients with borderline personality disorder using standard approaches. Traditional CBT told these patients their thoughts were distorted. But for people experiencing overwhelming emotional pain, hearing that their reality was somehow "wrong" felt invalidating and often made things worse.
Linehan developed DBT by combining cognitive-behavioural principles with Eastern mindfulness practices. The word "dialectical" refers to holding two seemingly opposite truths simultaneously. You can accept yourself exactly as you are AND still work toward meaningful change. You can feel devastating emotional pain AND recognize that the pain will pass.
The Four DBT Skills Modules
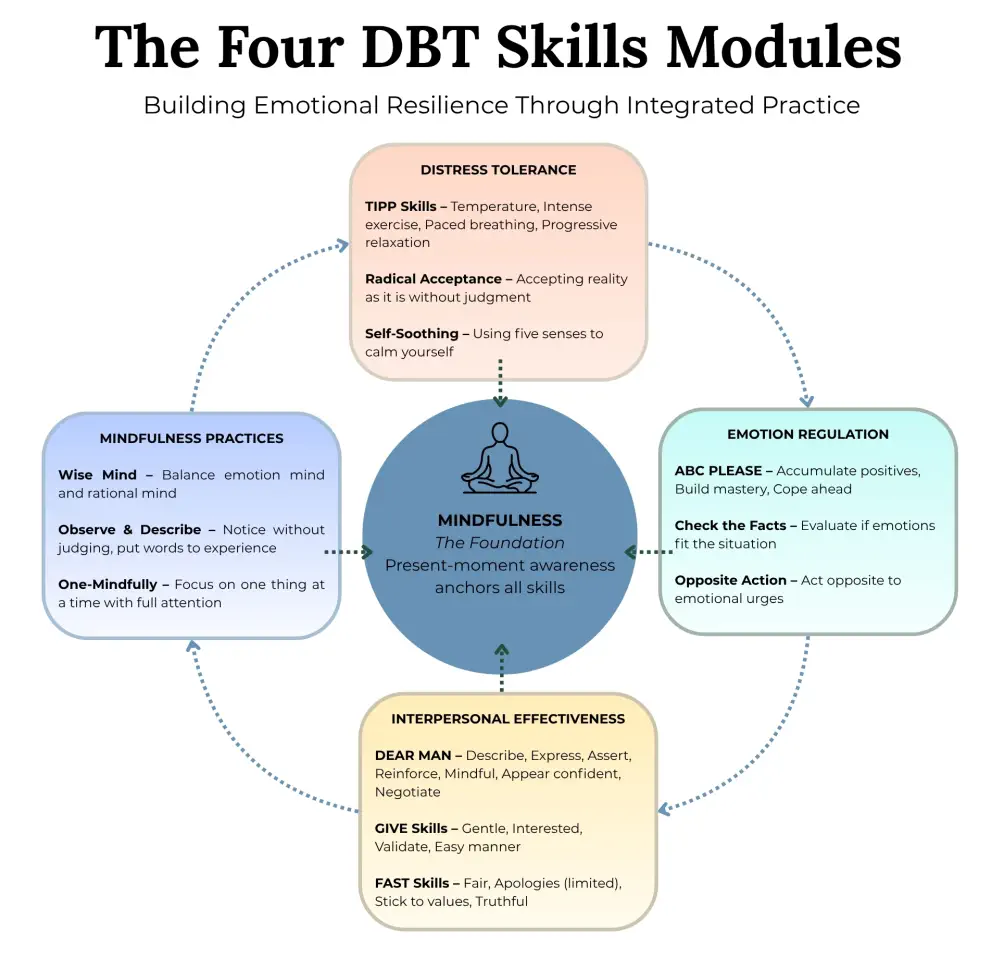
DBT teaches four interconnected skill sets that work together to create emotional stability:
Mindfulness forms the foundation of everything else. You learn to observe thoughts and feelings without judging them. When anger surges, you notice it without immediately acting on it. This creates space between stimulus and response, giving you choices you didn't have before.
Distress tolerance builds your capacity to survive crises without making things worse. Instead of reaching for substances or self-harm during overwhelming moments, you learn techniques like holding ice cubes, taking cold showers, or using intense sensory experiences to ride out emotional waves.
Emotion regulation helps you manage intense feelings. You learn to identify what you're actually feeling (often harder than it sounds), recognize what triggers certain emotions, and reduce vulnerability to emotional hijacking through basic self-care like adequate sleep and nutrition.
Interpersonal effectiveness teaches you to maintain relationships while respecting your own needs. How do you ask for what you want without damaging relationships? How do you say no without crippling guilt? These skills prove invaluable for anyone whose emotions historically sabotaged their connections with others.
DBT Treatment Structure
Standard dialectical behavioural therapy requires more time commitment than CBT. Treatment typically lasts six months to a year, although it may be longer in some cases. The structure includes:
- Individual therapy sessions happen weekly for about an hour. Here, you work through personal challenges with your therapist, applying DBT skills to specific situations in your life.
- Group skills training meets weekly for one to two hours. Unlike traditional group therapy, where you process emotions, skills groups focus on teaching. You learn specific techniques, practice them with peers, and troubleshoot obstacles. The group setting provides a safe space to rehearse interpersonal skills before trying them in real relationships.
- Phone coaching offers real-time support between sessions. When you're in crisis and need guidance applying skills, you can contact your therapist briefly for coaching. This bridges the gap between weekly sessions and real-life application.
- Therapist consultation teams ensure your treatment providers support each other effectively. DBT recognizes that working with intensely emotional clients can be draining. Regular team meetings prevent burnout and maintain treatment quality.
The Difference Between CBT and DBT
While DBT evolved from CBT principles, significant differences shape how each therapy approaches treatment. Recognizing these distinctions helps determine which approach might work better for specific challenges.
| Aspect | Cognitive Behavioural Therapy | Dialectical Behavioural Therapy |
| Primary Focus | Changing negative thought patterns | Regulating intense emotions |
| Core Philosophy | Logic and rational thinking (Socratic Method) | Acceptance AND change (mindfulness-based) |
| Treatment Duration | Short-term: 12-16 weeks typically | Longer-term: 6 months to 1+ year |
| Session Format | Primarily individual sessions | Individual therapy + group skills training |
| Approach to Emotions | Challenges emotional responses as potentially distorted | Validates emotions while teaching regulation |
| Between-Session Support | Homework assignments | Phone coaching available |
| Goal Orientation | Highly specific, measurable goals | A broader focus on building a life worth living |
| Therapeutic Relationship | Collaborative but primarily educational | Emphasizes validation and acceptance |
| Best Suited For | Anxiety, depression, phobias, OCD, PTSD | BPD, chronic suicidal ideation, self-harm, emotional dysregulation |
CBT vs DBT for Treating Specific Illnesses
Research consistently shows that certain mental health conditions respond better to specific therapeutic approaches. Matching the right therapy to the right condition dramatically improves outcomes.
Depression and Anxiety Disorders
CBT remains the gold standard for depression and generalized anxiety. Identifying and challenging negative automatic thoughts directly targets the cognitive patterns driving these conditions.
Someone with depression might think, "I'm a burden to everyone around me." CBT helps examine this belief critically. What evidence supports this thought? What contradicts it? Usually, the person discovers they're far less burdensome than depression convinces them they are.
For anxiety, CBT's structured exposure techniques prove particularly powerful. Gradually facing feared situations while learning that catastrophic predictions rarely materialize builds lasting confidence.
Meta-analyses show CBT achieving 50-60% success rates for depression and anxiety disorders. Effects often endure long after treatment ends because people learn skills they continue applying independently.
Borderline Personality Disorder
DBT was specifically created for borderline personality disorder and remains the only evidence-based treatment for this challenging condition.
People with BPD experience emotions far more intensely than others. Joy feels ecstatic. Rejection feels annihilating. These intense emotional swings, coupled with fears of abandonment, create chaotic relationships and sometimes dangerous behaviours.
Traditional CBT often backfires with BPD. Telling someone their intense fear of abandonment is "distorted thinking" feels invalidating and can trigger emotional crises. DBT instead acknowledges that, given their history and emotional sensitivity, these fears make complete sense. AND they can learn skills to manage them more effectively.
Research shows remarkable outcomes: up to 77% of people no longer meet BPD diagnostic criteria after one year of DBT. Rates of self-harm, suicide attempts, and psychiatric hospitalizations all decrease significantly.
Obsessive-Compulsive Disorder and PTSD
CBT, particularly its specialized variants, works exceptionally well for OCD and PTSD.
For OCD, Exposure and Response Prevention (a CBT technique) systematically exposes people to anxiety-triggering situations while preventing compulsive responses. Someone terrified of contamination might touch a "dirty" doorknob and resist washing their hands. Anxiety eventually decreases naturally, breaking the obsessive-compulsive cycle.
For PTSD, CBT-based approaches help process traumatic memories while challenging unhelpful beliefs about safety and self-blame. Prolonged Exposure therapy and Cognitive Processing Therapy both show strong evidence for reducing PTSD symptoms.
Substance Use Disorders
Both therapies show effectiveness for addiction treatment, though they target different aspects.
CBT helps identify triggers and develop alternative coping strategies. It examines the thought patterns leading to substance use ("I can't handle this stress sober") and challenges them systematically. This approach works particularly well when addiction stems from specific triggering situations or faulty beliefs about substances.
DBT addresses the emotional dysregulation often underlying addiction. Many people use substances to escape overwhelming emotions that they lack the skills to tolerate. Teaching distress tolerance and emotion regulation provides healthier alternatives to reaching for substances during emotional crises.
At treatment centres like the Canadian Centre for Addictions, therapists often combine elements of both approaches based on individual needs. Someone might use CBT techniques for identifying high-risk situations while applying DBT skills for managing cravings during emotionally intense moments.
Self-Harm and Chronic Suicidal Ideation
DBT proves most effective for these dangerous behaviours. The therapy was literally created to address them.
Standard CBT can feel dismissive to someone experiencing suicidal thoughts. Being told their thinking is distorted when they feel genuine emotional agony often increases feelings of isolation. DBT instead validates that their pain is real and understandable while providing concrete skills to survive crises without self-destructive actions.
Distress tolerance skills specifically target these moments. When someone feels they can't survive another minute of emotional pain, DBT offers immediate strategies: intense sensory experiences, self-soothing techniques, pros and cons lists, and radical acceptance practices that help ride out the crisis.

CBT vs DBT for Mental Health
Choosing between CBT and DBT therapy ultimately depends on your specific challenges, treatment goals, and personal characteristics. Neither therapy represents a superior approach universally; each excels in different circumstances.
Consider CBT when:
- You struggle with specific anxiety disorders, depression, or phobias
- You respond well to logical, structured approaches
- You prefer shorter-term treatment with measurable goals
- Your primary challenges involve negative thinking patterns
- You're motivated by homework and between-session practice
Consider DBT when:
- You experience intense emotional swings that feel uncontrollable
- Relationships repeatedly suffer due to emotional reactivity
- You engage in self-harm or have chronic suicidal thoughts
- Standard therapy hasn't worked or felt invalidating
- You're willing to commit to longer-term, intensive treatment
Many people benefit from elements of both approaches. A therapist might use CBT techniques for specific anxiety symptoms while incorporating DBT mindfulness skills for overall emotional regulation. The best treatment matches the therapeutic approach to individual needs rather than forcing everyone through identical protocols.
Recovery from addiction or mental health challenges rarely follows a straight path. Both cognitive behavioural therapy and dialectical behavioural therapy offer powerful tools for building lives free from substances and emotional chaos. Knowing the difference between CBT and DBT empowers you to advocate for treatment approaches that resonate with your specific situation.
FAQ
What is the main difference between CBT and DBT?
The primary difference between CBT and DBT lies in their focus areas. CBT targets negative thought patterns, teaching you to identify and challenge distorted thinking. DBT focuses on emotional regulation and distress tolerance, teaching skills to manage intense emotions without destructive behaviours. Both therapies share cognitive-behavioural foundations but apply them through different lenses.
Can I do both CBT and DBT at the same time?
Yes, many treatment programs incorporate elements of both therapies. You might use CBT techniques for specific anxiety symptoms while applying DBT skills for emotional regulation. Full standard DBT requires a significant time commitment, so attempting both complete programs simultaneously may prove impractical. Discuss with your therapist which combination best serves your needs.
How long does each therapy typically last?
Cognitive behavioural therapy usually runs 12 to 16 weeks with weekly sessions. Dialectical behavioural therapy requires longer commitment, typically six months to one year, sometimes longer. DBT's additional group skills component and extended structure account for the longer timeline. Treatment duration varies based on symptom severity and individual progress.
Which therapy works better for addiction?
Both show effectiveness for addiction, but for different reasons. CBT helps identify triggers and challenge beliefs about substance use. DBT addresses emotional dysregulation that often underlies addictive behaviours. Many addiction treatment centres combine both approaches. CBT targets specific high-risk situations while DBT provides skills for managing intense cravings and emotional states.
Is DBT only for borderline personality disorder?
No, though DBT was originally developed for borderline personality disorder. Research now supports its effectiveness for eating disorders, substance abuse, depression, PTSD, and any condition involving emotional dysregulation or self-destructive behaviours. The core skills of mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness benefit many different mental health challenges.
Do I need a diagnosis to receive CBT or DBT?
Not necessarily. While formal diagnosis helps guide treatment planning, many people benefit from these therapies without meeting full diagnostic criteria. If you struggle with anxiety, depression, emotional regulation, or unhelpful thinking patterns, these approaches may help regardless of diagnostic labels. Consult with a qualified therapist to determine which approach suits your specific situation.
Article sources
- Beck, A.T., et al. (1979). "Cognitive therapy of depression." The Guilford Press. Available at: https://www.guilford.com/books/Cognitive-Therapy-of-Depression/Beck-Rush-Shaw-Emery/9780898629194
- Linehan, M.M., et al. (1991). "Cognitive-behavioral treatment of chronically parasuicidal borderline patients." Archives of General Psychiatry, 48(12), 1060-1064. Available at: https://pubmed.ncbi.nlm.nih.gov/1845222/
- Hofmann, S.G., et al. (2012). "The efficacy of cognitive behavioral therapy: A review of meta-analyses." Cognitive Therapy and Research, 36(5), 427-440. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC3584580/
- May, J.M., Richardi, T.M., & Barth, K.S. (2016). "Dialectical behavior therapy as treatment for borderline personality disorder." Mental Health Clinician, 6(2), 62-67. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC6007584/
- Panos, P.T., et al. (2014). "Meta-analysis and systematic review assessing the efficacy of Dialectical Behavior Therapy (DBT)." Research on Social Work Practice, 24(2), 213-223. Available at: https://journals.sagepub.com/doi/10.1177/1049731513503047
- Carpenter, J.K., et al. (2018). "Cognitive behavioral therapy for anxiety and related disorders: A meta-analysis of randomized placebo-controlled trials." Depression and Anxiety, 35(6), 502-514. Available at: https://pubmed.ncbi.nlm.nih.gov/29451967/
- Linehan, M.M. (2015). "DBT Skills Training Manual." The Guilford Press, Second Edition. Available at: https://www.guilford.com/books/DBT-Skills-Training-Manual/Marsha-Linehan/9781462516995
- Oud, M., et al. (2019). "Effectiveness of CBT for children and adolescents with depression: A systematic review and meta-regression analysis." European Psychiatry, 57, 33-45. Available at: https://pubmed.ncbi.nlm.nih.gov/30658278/
- Stiglmayr, C., et al. (2014). "Effectiveness of dialectic behavioral therapy in routine outpatient care: The Berlin Borderline Study." Borderline Personality Disorder and Emotion Dysregulation, 1, 20. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC4579518/
- Cuijpers, P., et al. (2013). "A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments." The Canadian Journal of Psychiatry, 58(7), 376-385. Available at: https://pubmed.ncbi.nlm.nih.gov/23870719/





