We offer medical detox and multiple addiction treatment options in our
luxury treatment centres in Port Hope, Cobourg, and Ottawa.
What Are the 6 Stages of the Change Model?
The stages of change model, also called the transtheoretical model, outlines six distinct phases people move through when modifying their behaviour: precontemplation, contemplation, preparation, action, maintenance, and termination. This framework helps individuals and treatment providers understand where someone stands in their readiness to change, particularly when addressing addiction recovery.

Key Takeaway:
- How Two Psychologists Discovered Why Some People Change While Others Stay Stuck — The late 1970s research that revealed success came from doing the right things at the right time, not from willpower alone
- The Six Distinct Stages and What Each One Feels Like — From complete denial to long-term maintenance, you'll recognize exactly where you are in your own change process
- Why Stage 4 Carries the Highest Relapse Risk (And How to Navigate It) — The visible change phase surprises many with its challenges during the critical first 90 days
- The Controversial Sixth Stage That Addiction Experts Debate — Whether true "termination" exists for addiction recovery, or if maintenance continues indefinitely
- Stage-Matched Strategies That Triple Your Success Rates — Verified research showing how matching interventions to readiness dramatically improves outcomes
How Did the Stages of Change Model Begin?

The Smoking Cessation Studies
Psychologists James Prochaska and Carlo DiClemente developed the stages of change model in the late 1970s while studying smoking cessation. They interviewed hundreds of people trying to quit cigarettes. Some succeeded on their first try. Others failed repeatedly. The most revealing discovery? Successful quitters weren't doing anything particularly different—they were doing the right things at the right time.
Traditional psychology in that era ignored preparation. Researchers focused exclusively on what happened after someone decided to quit. This missed the entire mental journey leading up to that decision. Prochaska and DiClemente recognized they needed to map the complete territory of change.
From Observation to Framework
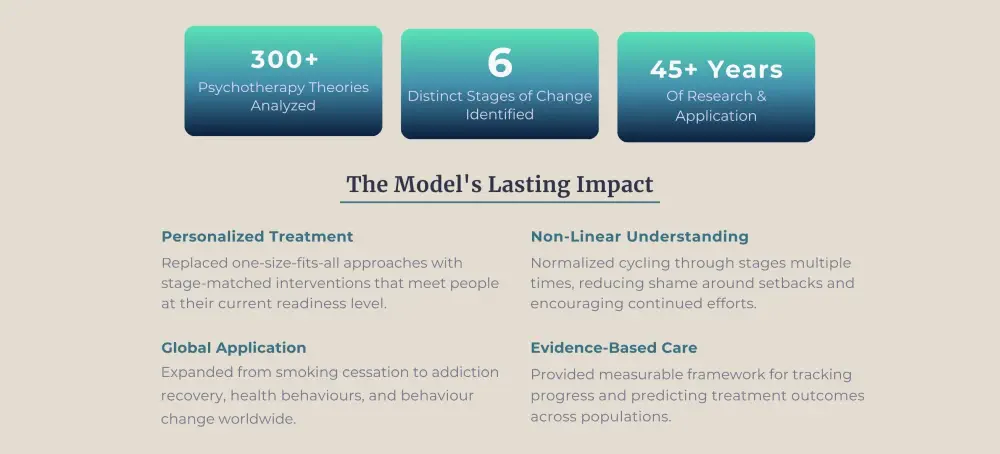
The researchers analyzed over 300 different psychotherapy theories searching for common patterns. None adequately explained why some people changed while others didn't. The breakthrough came from listening to regular people describe their experiences.
Someone in denial needed education and awareness. Someone ambivalent needed help resolving internal conflicts. Someone ready to act needed practical strategies. Matching support to readiness level became the key insight. The model shifted treatment philosophy from "fixing resistant patients" to "meeting people where they are."
Expansion Beyond Smoking
By the 1990s, the transtheoretical model had proven effective for numerous behaviours beyond smoking. Weight management, exercise adoption, and substance use treatment—the stages remained consistent across different challenges. Today, the model guides addiction recovery programs throughout Canada and worldwide, helping providers tailor interventions to individual readiness.
What Are the Six Stages of the Transtheoretical Model?

Stage 1: Precontemplation
The Denial Phase
Precontemplation means you don't recognize your behaviour as problematic. Plans to change within the next six months don't exist. Friends and family might see issues clearly. You don't.
What Maintains This Stage
In addiction recovery, this looks like someone insisting they can stop drinking anytime, despite regular blackouts. They minimize consequences. They blame external factors. "I only drink because my job stresses me out." Denial operates at full strength during this stage.
Four subtypes exist within precontemplation:
- Reluctance (lack of knowledge)
- Rebellion (hostility toward being told what to do)
- Resignation (feeling overwhelmed)
- Rationalization (creating elaborate justifications)
Each requires different intervention strategies.
External Pressure vs. Internal Readiness
People in precontemplation arrive at treatment through external pressure—court orders, employer ultimatums, family interventions. They show up physically but remain mentally uncommitted to change. This creates the challenge treatment providers face: building internal motivation when none exists yet.
Stage 2: Contemplation
The Ambivalence Stage
Awareness arrives without commitment in contemplation. You recognize your behaviour causes problems. You're thinking about changing within the next six months. But ambivalence runs deep.
The Decisional Balance Shift
The defining characteristic — weighing pros and cons endlessly without taking action.
"I know I should quit, but..." becomes your constant refrain. You see both sides clearly. This creates paralysis, not movement.
Research shows that in precontemplation, perceived cons of changing outweigh the pros. During contemplation, this balance begins shifting. The pros and cons become roughly equal, creating the stuckness that defines this stage.
How Long People Stay Stuck
Someone struggling with opioid addiction might acknowledge they've lost relationships and job opportunities. They research treatment options. They talk about getting help, make plans—then postpone actually doing anything. Ambivalence keeps them stuck in this stage, sometimes for years. Some people spend their entire lives contemplating change without ever moving forward.

Stage 3: Preparation
The Planning Phase
Planning replaces thinking in the preparation stage. You intend to take action within the next month. The question shifts from 'whether' to 'how'.
Small Steps Forward
This stage involves concrete steps. Calling treatment centres. Attending support group meetings. Telling supportive friends about your plans. You're gathering resources and building a strategy for change.
The key difference from contemplation — You've made a commitment, even if anxiety accompanies it. People in preparation have usually set a quit date or start date. They're making final adjustments before launching into action.
Vulnerability to Setbacks
In addiction recovery, someone might dispose of their supply, research detox facilities, or schedule an appointment with an addiction counsellor. Small actions demonstrate genuine readiness. Anxiety usually accompanies these preparations.
Preparation carries its own risks. Some people get stuck here, endlessly preparing without ever acting. Others rush through preparation inadequately, leading to action-stage failures. The sweet spot involves thorough preparation followed by committed action.
Stage 4: Action
The Visible Change Phase
Action means you've modified your behaviour within the past six months. You're actively working on change, implementing your plans, following through on commitments.
This is the stage most visible to others. You've entered treatment, attended therapy sessions, and stopped using substances. Your daily routines look different. You're building new habits and coping strategies.
Why This Stage Has the Highest Relapse Risk
The action phase demands the most time and energy. You're learning to manage triggers, handle cravings, and rebuild your life without substances. This stage carries a high relapse risk because you're still establishing new patterns as old habits pull strongly.
The first 90 days prove particularly difficult. Neural pathways associated with addiction remain strong. New healthy patterns haven't solidified yet. Environmental cues trigger automatic responses that require conscious effort to override.
The Role of Support Systems
Success in action depends heavily on support structures. People trying to change alone face dramatically higher failure rates than those with professional help, peer support, and family involvement. The action stage isn't about willpower—it's about accessing the right resources at the right time.
Stage 5: Maintenance
The Consolidation Phase
Six months of sustained behaviour change mark the beginning of maintenance. Initial challenges have been worked through. New routines are established. The focus now shifts to preventing relapse and strengthening recovery.
Confidence grows during this stage. The new behaviour feels more automatic. It requires less conscious effort. Triggers still exist, but effective management strategies have been developed.
The Danger of Overconfidence
Someone in maintenance might attend regular therapy sessions, participate in support groups, practice stress management techniques, and maintain healthy boundaries. The goal is consistent progress and quick recovery from occasional slips.
A risk emerges in maintenance: complacency. People feel so confident that they stop doing the things that got them there. They skip support meetings. They reduce therapy frequency too quickly. They convince themselves they're "cured" and no longer need help.
Long-Term Maintenance Strategies
Research indicates that maintenance can last from six months to five years before people feel fully confident in their new behaviour. For addiction recovery, many experts suggest viewing maintenance as a lifelong commitment, not a temporary phase to push through.
Stage 6: Termination
The Controversial Final Stage
Termination represents total confidence in your new behaviour. You experience zero temptation to return to old patterns. Your changed behaviour has become completely automatic and integrated into your identity.
Does Termination Exist for Addiction?
Most experts question whether true termination exists in recovering from addiction. Unlike quitting caffeine or starting an exercise routine, addiction involves neurological changes that create lasting vulnerability. Many people in long-term recovery prefer thinking of themselves as always in maintenance, not terminated.
Brain imaging studies show that addiction creates permanent changes in neural pathways. These pathways weaken over time without use, but they never completely disappear. This is why someone sober for decades can still experience cravings under stress.
Relapse as an Alternative Sixth Stage
Some models replace termination with relapse as the sixth stage, acknowledging that setbacks happen frequently in recovery. Relapse isn't failure—it's information about what needs adjustment in your plan.
When relapse occurs, most people return to contemplation or preparation, not all the way back to precontemplation. They've learned from previous attempts. Each cycle through the stages builds skills and insights that make the next attempt more likely to succeed.

Why Does the Stages of Change Model Matter for Addiction Recovery?
Stage-Matched Interventions
Comprehending these six stages reveals why the transtheoretical model revolutionized addiction treatment. Research consistently shows that matching interventions to someone's current stage produces better outcomes than generic treatment plans.
Someone in precontemplation benefits from consciousness-raising exercises and educational materials about consequences. Pushing them toward action creates resistance and treatment dropout. Conversely, someone in preparation or action wastes valuable time with consciousness-raising; they need concrete skills and relapse prevention strategies.
The Cost of Mismatched Treatment
Treatment centres that ignore stage readiness face predictable patterns. Precontemplation clients forced into action-focused programs often leave treatment early or sabotage their own progress. Action-ready clients stuck in contemplation-focused group therapy lose motivation waiting for others to "get ready."
Research demonstrates striking differences in outcomes. A study in cardiac patients showed that only 22% of precontemplators and 43% of contemplators succeeded in quitting smoking after six months when placed in action-oriented programs. By contrast, 76% of individuals already in the action stage succeeded with the same interventions. The Canadian Centre for Addictions incorporates stage assessment into intake procedures, ensuring each person receives interventions aligned with their current readiness.
Reducing Shame Through Understanding
The cyclical view reduces shame around relapse. Research shows that most successful changers cycle through the stages three to four times before achieving lasting change. Each cycle provides learning opportunities instead of evidence of failure.
This reframing matters enormously. People who view relapse as personal failure often spiral into deeper addiction. Those who view it as valuable data about what didn't work return to active change efforts more quickly. The model teaches that relapse means you've learned which stage-specific skills you still need to develop.
How Can You Apply This Model to Your Recovery?
Begin with an honest assessment. Where do you stand right now? Still questioning whether you have a problem? Weighing pros and cons? Actively working on change?
Answer these questions:
- Do you believe your substance use is problematic? (No = precontemplation; Yes, but... = contemplation).
- Have you made concrete plans to change within the next month? (Yes = preparation).
- Have you already stopped or significantly reduced use? (Within 6 months = action; Over 6 months = maintenance).
Stage-Specific Strategies
- Precontemplation stage: Increase awareness. Keep a journal tracking how behaviour affects your life. Notice patterns without judgment. Talk to trusted people about their observations. Read educational materials about addiction. The goal isn't to change yet—it's building awareness that change might be needed.
- Contemplation stage: Create a decisional balance sheet. List every reason to change and every reason to stay the same. Notice which side feels heavier emotionally. Explore the specific concerns keeping you stuck. What would need to be different for you to move toward preparation? What resources would help you feel ready?
- Preparation stage: Build a support system. Research treatment options in your area. Tell supportive people about plans. Set a specific date to begin taking action. Create a detailed plan addressing: who will support you, what triggers to avoid, where you'll go for help, when you'll start, and how you'll handle cravings.
- Action stage: Follow the treatment plan consistently. Develop daily routines supporting recovery. Learn and practice new coping skills. Stay connected to supportive people and environments. Track your progress daily. Celebrate small wins. Reach out immediately when struggling.
- Maintenance stage: Continue recovery activities even when they feel unnecessary. Stay alert to warning signs of relapse. Celebrate progress while remaining realistic about ongoing vulnerability. Update your relapse prevention plan as life circumstances change. Mentor others earlier in recovery—teaching reinforces your own learning.
Working with Treatment Providers
At the Canadian Centre for Addictions, our treatment programs align with the stages of change model. We assess where you are in your recovery and provide stage-appropriate interventions. Our 95.6% success rate reflects this personalized care for addiction recovery.
Communicate openly with your treatment team about where you feel you are. Good providers will adjust interventions when you move between stages. Recovery isn't linear—your needs will change as you progress.
FAQ
How long does each stage last?
Stage duration varies dramatically between individuals. Some people spend years in contemplation, while others move quickly through preparation into action. There's no predetermined timeline; your pace depends on readiness, support, circumstances, and the specific behaviour change you're attempting.
Can you skip stages in the transtheoretical model?
Skipping stages usually leads to problems. Someone who jumps from precontemplation directly to action without contemplation or preparation struggles to maintain changes. The earlier stages build the groundwork and motivation needed for lasting change.
Is relapse a failure of the stages of change model?
Relapse isn't failure—it's part of normal change for many people. Most successful changers cycle through the stages multiple times. Each relapse provides information about triggers, vulnerabilities, and needed adjustments to your recovery plan.
How do treatment providers use this model?
Treatment providers assess your current stage and match interventions accordingly. Someone in contemplation receives motivational interviewing to resolve ambivalence. Someone in action gets concrete skills training and relapse prevention strategies. This stage-matched method improves addiction recovery outcomes significantly.
Does the stages of change model work for all addictions?
Yes, the transtheoretical model applies to all types of addiction recovery—alcohol, opioids, stimulants, gambling, or other behaviours. The stages remain consistent across different substances and behaviours, though specific interventions might vary based on what you're changing.
Article sources
- Prochaska, J.O., & DiClemente, C.C. (1983). "Stages and processes of self-change of smoking: toward an integrative model of change." Journal of Consulting and Clinical Psychology, 51(3), 390-395. Available at: https://psycnet.apa.org/record/1983-25938-001
- Krebs, P., Prochaska, J.O., & Rossi, J.S. (2010). "A meta-analysis of computer-tailored interventions for health behavior change." Preventive Medicine, 51(3-4), 214-221. Available at: https://pubmed.ncbi.nlm.nih.gov/20558196/
- Norcross, J.C., Krebs, P.M., & Prochaska, J.O. (2011). "Stages of change." Journal of Clinical Psychology, 67(2), 143-154. Available at: https://pubmed.ncbi.nlm.nih.gov/21157930/
- Prochaska, J.O., DiClemente, C.C., & Norcross, J.C. (1992). "In search of how people change: applications to addictive behaviors." American Psychologist, 47(9), 1102-1114. Available at: https://psycnet.apa.org/record/1993-01846-001
- Velicer, W.F., et al. (2007). "Enhancing motivation for change in problem drinking: a controlled comparison of two therapist styles." Journal of Consulting and Clinical Psychology, 75(4), 618-629. Available at: https://pubmed.ncbi.nlm.nih.gov/17663615/





