We offer medical detox and multiple addiction treatment options in our
luxury treatment centres in Port Hope, Cobourg, and Ottawa.
What Is Cross Addiction?
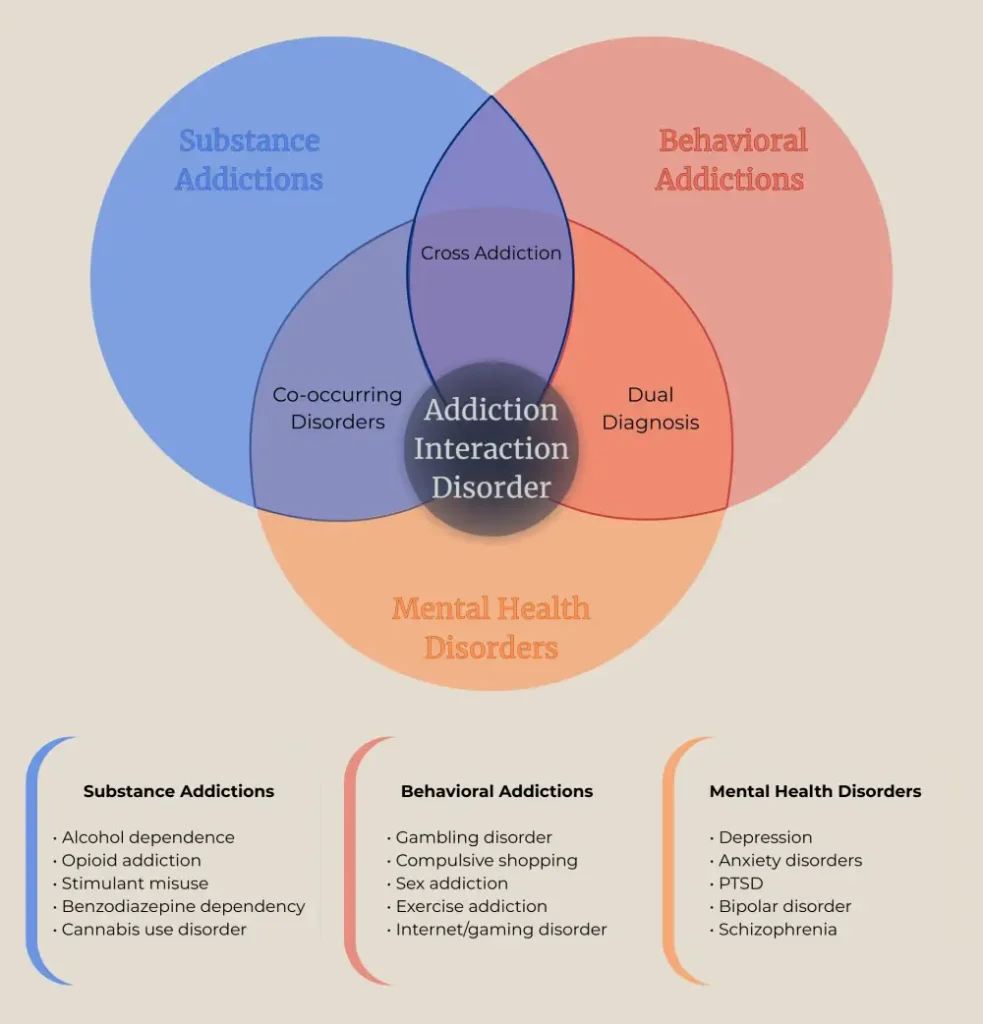
Cross addiction happens when someone acquires a new dependency while recovering from another, or struggles with multiple addictions simultaneously. The term also appears as addiction transfer or addiction interaction disorder in clinical settings. Your brain doesn't distinguish between the high from substances and the rush from certain behaviours. Both flood your reward system with dopamine, creating similar patterns of compulsion and loss of control.
This affects more Canadians than you might expect. Research from Alberta shows that 40% of adults reporting problems with one addictive behaviour actually struggle with two or more. These patterns can destroy recovery progress just as thoroughly as relapsing on your original substance.
Key Takeaway:
- How your brain's reward system stays vulnerable long after you stop using substances, creating unexpected openings for entirely different addictive behaviors to take hold.
- Which addiction transitions happen most frequently — from alcohol to prescription anxiety medications, opioids to other pills, and substances to behavioral addictions like gambling.
- Hidden factors beyond brain chemistry that drive cross addiction, including unresolved trauma, genetic vulnerabilities, and environmental triggers that persist throughout recovery.
- Early warning signs that distinguish normal recovery adjustments from emerging cross addiction patterns, giving you the power to intervene before consequences escalate.
- Why treating multiple dependencies simultaneously produces better outcomes than the traditional approach of addressing one addiction at a time.
How Does Cross Addiction Develop?
Your brain's reward system operates like a thermostat, constantly adjusting to maintain balance. Prolonged substance use or compulsive behaviours reset this balance point. The dopamine receptors become less sensitive, requiring increasingly intense stimulation to feel normal, let alone good.

When you stop using your primary substance, the underlying dysfunction remains. Your brain still craves that dopamine surge. Any activity that triggers the reward system (gambling, shopping, eating, sex, even exercise) can fill that void temporarily. The addictive patterns transfer without disappearing.
Two Ways Addictions Interact
Addiction interaction disorder manifests in two distinct ways. Some people battle multiple addictions concurrently, switching between substances or behaviours based on availability, mood, or circumstance. Others experience sequential addictions, where one dependency replaces another over months or years. A recovered alcoholic might become dependent on benzodiazepines prescribed for anxiety. Someone who quits smoking could acquire compulsive eating patterns.
Which Cross Addiction Combinations Appear Most Frequently?
Alcohol to Prescription Medications
Alcohol dependence frequently transitions into prescription medication misuse. Benzodiazepines prescribed for anxiety during early sobriety carry their own addiction potential. Opioid painkillers given after surgery or injury present similar risks. These medications affect the same brain receptors that alcohol does, making the transition feel natural, almost inevitable.
Drug users may discover that gambling fills the same need their substance did. The anticipation, the rush, the escape from daily stress—poker machines or sports betting provide all of it. One Alberta study found that 58% of people with gambling disorders also struggled with substance dependencies at some point.
Exercise and Stimulant Connections
Behavioural addictions can precede substance use, too. Someone who exercises compulsively might start using stimulants to enhance performance or maintain energy levels. The line blurs between dedication and obsession until stimulants become necessary, not optional.
Food as Gateway or Substitute
Food represents another common substitution. After bariatric surgery, some patients who can no longer binge eat turn to alcohol or drugs. Their brain still needs that dopamine hit; they've simply changed the delivery method. The underlying compulsion persists regardless of the specific addictive behaviour.

What Causes Cross-Addiction Beyond Brain Chemistry?
Neurological dysfunction explains part of the picture. Trauma explains much of the rest. Childhood abuse, neglect, violence, or other painful experiences create wounds that substances and compulsive behaviours temporarily soothe. Stopping one addiction doesn't heal those wounds. Without addressing the trauma directly, people naturally seek other ways to cope with the pain they've carried for years.
Mental Health Conditions Increase Risk
Mental health conditions create additional vulnerability. Depression makes the world feel colourless and heavy. Anxiety turns ordinary situations into threats. PTSD keeps the past perpetually present. Substances and certain behaviours offer relief from these symptoms, which is why concurrent disorders appear so frequently. 282,000 Canadians experienced both mental health and substance issues simultaneously according to 2012 data.
Genetic Predisposition Matters
Genetic factors matter more than most people realize. Having a parent or sibling with addiction increases your risk substantially. Your brain may produce less dopamine naturally or handle it differently, making you more vulnerable to any activity that artificially boosts these levels. Family history doesn't guarantee you'll acquire addiction interaction disorder, but it stacks the deck against you.
Environmental Stressors Never Disappear
Environmental triggers persist long after treatment ends. The stress of daily life doesn't disappear because you completed rehab. Financial pressure, relationship conflicts, work demands—these challenges can overwhelm newly built coping skills. Without healthy stress management techniques, reverting to addictive patterns becomes the path of least resistance, even if the specific addiction changes.
How Can You Prevent Cross-Addiction During Recovery?
Awareness creates your first line of defence. Knowing you're vulnerable to acquiring new addictions changes how you handle recovery.
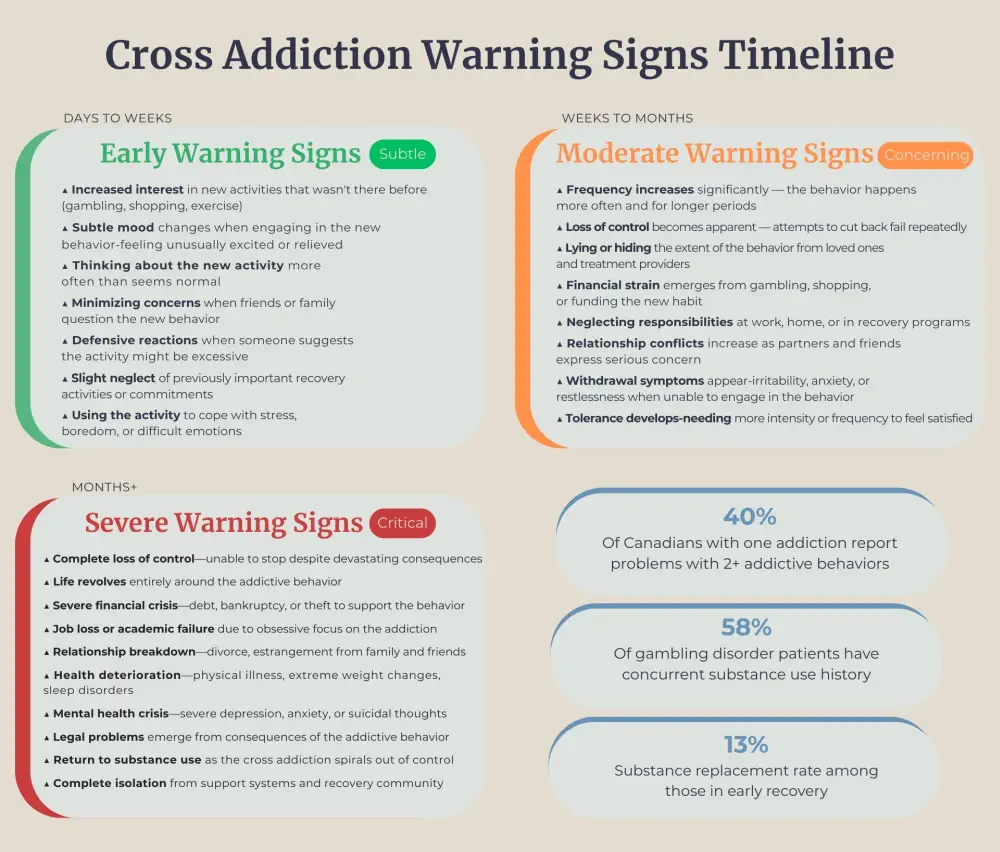
Warning signs: spending increasing time and money on activities, feeling unable to stop even with negative consequences, and hiding behaviours from loved ones.
Recognition allows early intervention before patterns solidify.
Address Root Causes, Not Just Symptoms
Treatment must address underlying causes, not just the substance itself. Programs that focus solely on stopping alcohol use or drug consumption miss the point. Why did you start using? What pain were you trying to escape? Which emotional regulation skills do you lack? Answering these questions honestly (with professional help) reduces the likelihood of simply switching addictions.
Build Healthy Coping Skills
Building genuine coping mechanisms takes time and practice. Therapy teaches you to sit with uncomfortable feelings without immediately seeking relief. You learn that anxiety eventually decreases on its own if you don't interfere. Boredom passes. Sadness doesn't last forever. These truths seem obvious until you're experiencing the emotions yourself.
Connection Prevents Relapse
Support systems provide accountability and connection. Regular check-ins with a counselor or sponsor help identify concerning patterns early. Support groups connect you with others who understand the struggle without judgment. Isolation breeds addiction; connection prevents it. British journalist Johann Hari summarized years of research with one sentence: the opposite of addiction isn't sobriety, it's connection.
Monitoring your behaviours honestly requires brutal self-assessment.
- Are you gambling more frequently?
- Exercising to the point of injury?
- Shopping beyond your means?
- Eating compulsively?
These questions feel uncomfortable, but avoiding them allows cross-addiction to take root unchallenged.
Which Treatment Programs Specialize in Addiction Interaction Disorder?
Integrated treatment targeting multiple addictions simultaneously produces better outcomes than addressing issues separately. Your brain doesn't compartmentalize its dysfunction—alcohol dependence, gambling compulsion, and depression interact constantly. Treatment should mirror this reality.
Cognitive-Behavioural Methods Target Patterns
Cognitive-behavioural methods help identify thought patterns driving addictive behaviour across different substances and activities. You learn to recognize triggers regardless of their specific form. The urge to gamble and the craving for cocaine both stem from similar emotional states and thinking patterns. Treating the underlying pattern, not individual manifestations, creates lasting change.
Multiple Therapy Layers Address All Needs
Individual counselling provides space to explore trauma, shame, and emotional regulation challenges privately. Group therapy offers peer support and reduces isolation. Family therapy repairs relationships damaged by addiction and educates loved ones about realistic recovery expectations. No single intervention works alone; integrated care combines multiple strategies tailored to individual needs.
Programs at the Canadian Centre for Addictions
The Canadian Centre for Addictions addresses addiction interaction disorder through programs designed to identify and treat multiple dependencies. Our facilities in Port Hope and Cobourg, Ontario, provide medically supervised treatment in settings that support healing. Programs include trauma-focused therapy, skill-building workshops, and ongoing aftercare planning.
Success requires addressing physical, psychological, and social dimensions simultaneously. Medication-assisted treatment helps manage withdrawal and cravings. Counselling targets thought patterns and emotional triggers. Support groups rebuild social connections. Aftercare planning prepares you for challenges you'll face months after leaving treatment.

What Warning Signs Mean You Can't Handle Recovery Alone?
Recognizing you've acquired a new addiction feels devastating after working so hard to overcome the first one. That shame frequently delays seeking help, allowing the new dependency to strengthen. Don't wait until the consequences become severe.
Seek evaluation if you're spending increasing time or money on any activity. If you feel unable to stop even when wanting to. If loved ones express concern about changes in your behaviour. If you're lying or hiding activities from family members. These signs indicate the addictive behaviour has moved beyond casual interest into compulsive territory.
Self-managed recovery attempts frequently fail with cross-addiction because the underlying issues remain unaddressed. Professional treatment provides structure, accountability, and expertise that significantly improve recovery outcomes. At the Canadian Centre for Addictions, our treatment programs focus on treating the whole person, not just isolated symptoms.
FAQ
Is cross-addiction the same as having multiple addictions?
Cross addiction specifically refers to acquiring new addictions during or after recovering from another, or struggling with several addictions that interact and reinforce each other. Having multiple independent addictions without this interactive pattern differs slightly, though treatment methods overlap significantly.
How common is cross addiction in Canada?
Canadian research indicates approximately 40% of adults who report problems with one addiction also struggle with additional substances or behaviours. Among people seeking treatment for substance disorders, rates of concurrent behavioural addictions reach even higher percentages, particularly with gambling and compulsive behaviors.
Can behavioural addictions be as serious as substance addictions?
Behavioural addictions activate the same brain reward pathways and create similar patterns of compulsion, loss of control, and negative consequences. Gambling addiction causes financial devastation, relationship destruction, and increased suicide risk comparable to substance dependencies. The biological driver differs, but the damage remains equally severe.
Does treating one addiction prevent others from emerging?
Treatment focused only on stopping substance use without addressing underlying causes provides limited protection against acquiring new addictions. Thorough treatment targeting trauma, mental health conditions, and emotional regulation skills significantly reduces the risk of addiction interaction disorder emerging during recovery.
What's the difference between cross addiction and co-occurring disorders?
Co-occurring disorders refer to having both a mental health condition (depression, anxiety, PTSD) and a substance use disorder simultaneously. Cross addiction specifically involves multiple addictive behaviors or substances. Someone can have both (multiple addictions plus mental health conditions) which requires specialized integrated treatment methods.
Article sources
- el-Guebaly, N., et al. (2006). "Compulsive features in behavioural addictions: the case of pathological gambling." Addiction, 101(11), 1531-1537. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC2762921/
- Statistics Canada. (2014). "Concurrent mental and substance use disorders in Canada." Health Reports, 25(8). Available at: https://www150.statcan.gc.ca/n1/pub/82-003-x/2017008/article/54853-eng.htm
- Lorains, F.K., et al. (2011). "Prevalence of comorbid disorders in problem and pathological gambling: systematic review and meta-analysis of population surveys." Addiction, 106(3), 490-498. Available at: https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2021.659171/full
- Hari, J. (2015). Chasing the Scream: The First and Last Days of the War on Drugs. New York: Bloomsbury Publishing. The quote "The opposite of addiction isn't sobriety, it's connection" is attributed to Johann Hari from this work and his 2015 TED Talk "Everything you think you know about addiction is wrong."
- Grant, J.E., et al. (2010). "Introduction to Behavioral Addictions." American Journal of Drug and Alcohol Abuse, 36(5), 233-241. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3164585/
- Sussman, S., et al. (2011). "Prevalence of the Addictions: A Problem of the Majority or the Minority?" Evaluation & the Health Professions, 34(1), 3-56. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3134413/
- Health Canada. (2019). "Canadian Alcohol and Drugs Survey (CADS): Summary of results for 2019." Government of Canada. Available at: https://www.canada.ca/en/health-canada/services/canadian-alcohol-drugs-survey/2019-summary.html
- Potenza, M.N. (2006). "Should addictive disorders include non-substance-related conditions?" Addiction, 101(Suppl 1), 142-151. Available at: https://onlinelibrary.wiley.com/doi/10.1111/j.1360-0443.2006.01591.x





