We offer medical detox and multiple addiction treatment options in our
luxury treatment centres in Port Hope, Cobourg, and Ottawa.
Ottawa’s Teen Opioid Epidemic: What’s Changed since 2017
February 2017 marked a breaking point for Ottawa families. Chloe Kotval, just 14 years old, died after taking what she thought were prescription pills at a party. Her mother found her unresponsive in their Kanata home. Two days later, she was gone. Fentanyl had contaminated those pills—something neither Chloe nor her friends could have detected.

Seven years later, the numbers tell a darker story than anyone anticipated. The opioid epidemic that seemed to explode into public consciousness in 2017 has fundamentally reshaped how young people in Ottawa (and across Canada) encounter drugs, overdose, and death.
Key Takeaways:
- The 2017 panic focused on teens, but adults accounted for 94% of overdoses—what changed to make young people the fastest-growing victim demographic?
- Rising Teen Deaths — Opioid-related deaths among teens and young adults tripled between 2014 and 2021, with many victims not previously diagnosed with opioid use disorder.
- The Treatment Gap — Despite rising overdose deaths, treatment rates for opioid use disorder among young people have decreased, with stigma and lack of youth-focused services being key barriers.
- Depression, anxiety, and academic pressure drive teens toward opioids faster than any other factor—yet mental health services remain largely separate from addiction treatment.
- Signs of Opioid Use — Parents should be vigilant for physical and behavioural red flags, like constricted pupils, drowsiness, and secrecy, and act early if they suspect their child is using opioids.
What Sparked the 2017 Opioid Panic in Ottawa's Suburbs?
Back in 2017, panic spread faster than accurate information. Media coverage focused heavily on teenage victims, creating the impression that Ottawa's suburbs faced an unprecedented youth epidemic. Community meetings in Kanata drew hundreds of terrified parents. Naloxone kits flew off pharmacy shelves.
Yet the data painted a more nuanced picture. Ottawa paramedics responded to 101 opioid overdoses requiring naloxone in 2016, averaging four calls per week. Critically, only 5.6% of these cases involved patients aged 10-19. Adults in their 20s and 30s accounted for the vast majority of overdoses. Even seniors experienced more overdose calls than teenagers.
This doesn't diminish Chloe's death or the very real danger facing young people. What it reveals is how prescription opioids and illicit drugs contaminated with fentanyl created risks that crossed all age boundaries. Parents focused on their teens, but the crisis was already claiming lives across every demographic.
How Has the Drug Supply Changed Since 2017?
Seven years change everything in a drug crisis. What began as primarily prescription opioid misuse has become something far deadlier.
Fentanyl's Complete Takeover
In 2017, fentanyl contamination was emerging as a serious concern. Today, it dominates. Recent data shows that fentanyl directly contributed to 94% of opioid-related deaths among teens and young adults. That percentage actually increased during the COVID-19 pandemic, jumping from 84% before 2020 to even higher rates after.
Think about that shift. Nearly every teen or young adult who dies from opioids now has fentanyl in their system. This synthetic opioid—50 times stronger than heroin and 100 times stronger than morphine—has fundamentally altered the risk calculation. Someone experimenting once, trying what they believe is a prescription pill, faces lethal danger.
The Numbers That Should Alarm Every Parent
Between 2014 and 2021, opioid-related deaths among Ontario teens and young adults tripled. Read that again. Tripled. Emergency department visits related to opioid use quadrupled over the same period.
These numbers represent hundreds of young lives cut short. Families shattered. Futures erased.
Even more concerning: only about 50% of teens and young adults who died from opioid-related causes had an opioid use disorder diagnosis. This means half the deaths occurred among young people who weren't regular users. They might have experimented once at a party. Taken a pill to manage stress during exams. Used recreationally without understanding the contaminated supply they were accessing.
How Many People Are Affected By The Opioid Epidemic?
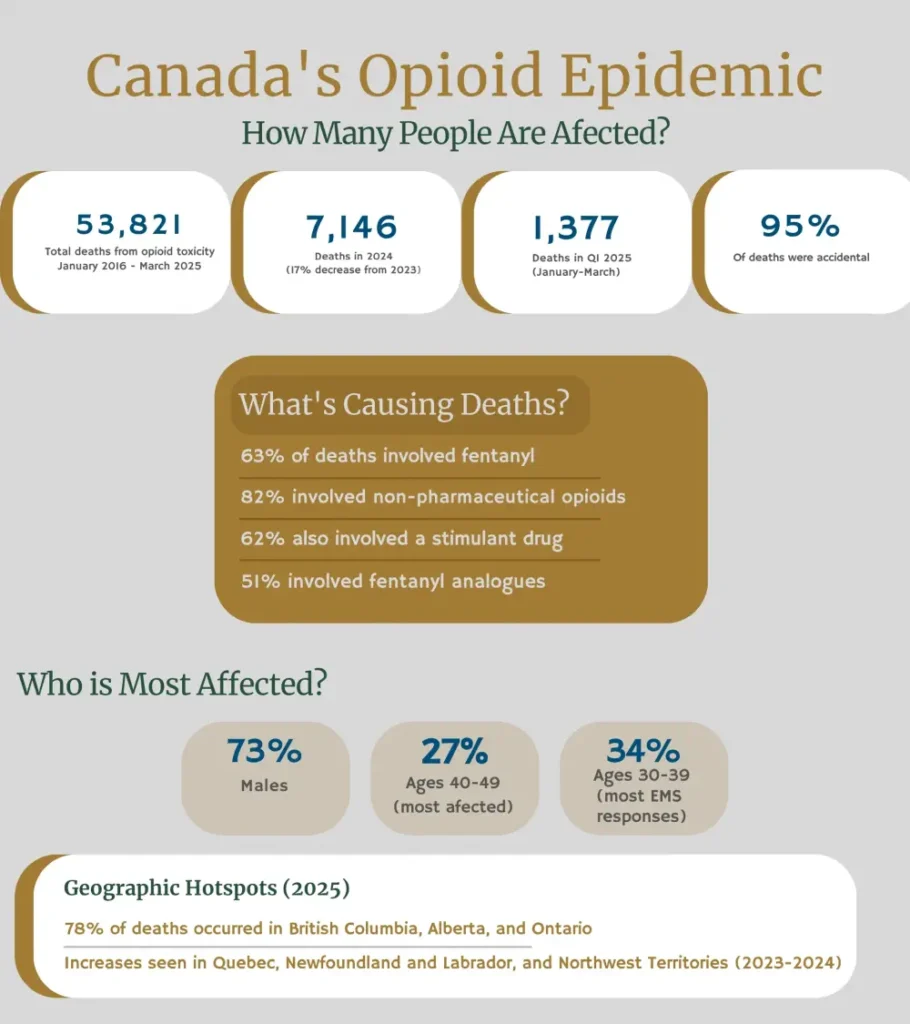
Across Canada, more than 53,000 apparent opioid toxicity deaths have been reported between January 2016 and March 2025. Males account for 73% of these deaths. The hardest-hit age group? People in their 40s, representing 27% of fatalities. But teens and young adults face rapidly increasing risks, with their death rates climbing faster than any other demographic.
Ontario, Alberta, and British Columbia together account for 78% of apparent opioid toxicity deaths. Ottawa sits within Ontario's data, reflecting provincial trends while also showing unique local patterns shaped by drug supply routes, harm reduction services, and community responses.
The Treatment Gap Grows Wider
Here's a statistic that defies logic: as opioid deaths among teens and young adults soared, treatment rates plummeted. Medications used to treat opioid use disorder (including methadone and buprenorphine) fell 50% among people aged 15-24 between 2014 and 2021.
Why? Multiple factors contribute. Stigma keeps young people from seeking help. Many fear parental reactions or legal consequences. Treatment programs designed for adults don't address adolescent needs. Waitlists stretch for months. Some communities lack youth-focused services entirely.
Only about one-third of teens and young adults with opioid use disorder who died had received any treatment in the previous year. Compare that to almost half of adults aged 25-44. Young people face the steepest barriers precisely when intervention could save their lives.
What Role Does Anxiety Play in Teen Substance Abuse?
The opioid epidemic and mental health challenges intertwine in ways that make both crises worse. Research consistently shows teens cite mental health struggles as primary reasons for opioid misuse.
Depression drives many young people toward drugs that promise numbness. Pills seem like a quick relief for anxiety disorders. When trauma survivors can't access appropriate therapy, many turn to self-medication instead. Academic pressure—the relentless push for perfect grades and college admission—leaves some teens desperate for anything that might ease the stress.
Focus groups with high school students revealed that anxiety, depression, and suicidal ideation ranked among the most commonly cited reasons for which peers misuse prescription opioids. One student explained it simply: "Maybe they have bad anxiety or something like that, and they think that it will help."
The COVID-19 pandemic amplified these mental health challenges. Isolation, disrupted education, family stress, and economic uncertainty—all contributed to deteriorating youth mental health. Not coincidentally, opioid deaths surged during this same period. The pandemic created conditions where vulnerable young people faced heightened risks on multiple fronts simultaneously.
The problem intensifies because young people often fail to understand addiction risk. They believe they're in control. They think they can stop anytime. They underestimate how quickly dependence develops.
Recognizing Signs of Opioid Addiction in Your Teen
Parents often miss early warning signs because they don't know what to look for. Signs of opioid addiction can be subtle at first, then escalate rapidly.
Physical Warning Signs
- Constricted pupils even in low light
- Drowsiness or nodding off at unusual times
- Slurred speech or slowed movements
- Unexplained weight loss or gain
- Changes in sleep patterns—either insomnia or sleeping far more than usual
- Frequent flu-like symptoms (which might actually be withdrawal)
- Coordination problems or unsteadiness
Behavioural Red Flags
- Stealing prescription medications from family members or friends
- Increased secrecy about activities and whereabouts
- New friend groups, especially if the teen is evasive about them
- Declining academic performance despite previous success
- Loss of interest in activities they once enjoyed
- Mood swings that seem extreme or unpredictable
- Financial problems—money disappearing, selling possessions, borrowing frequently
The Progression Pattern
Early-stage misuse might look like occasionally taking pills that weren't prescribed to them. Maybe they grab leftover painkillers after a family member's surgery. Perhaps they purchase pills at school.
As tolerance develops, they need higher doses to achieve the same effects. They might start crushing pills to snort or inject them. When prescription opioids become too expensive or hard to obtain, some teens turn to heroin as a cheaper alternative—never realizing it's likely contaminated with fentanyl.
The shift from casual use to daily dependence can happen frighteningly fast with opioids. What began as experimentation or stress relief transforms into a physical need.

What Parents Should Do If They Suspect Opioid Use
Immediate Steps
Don't wait for absolute proof before acting. If you suspect opioid use, trust your instincts. Approach your teen calmly rather than with anger. Accusations and punishment often drive the behaviour deeper underground. You want them to feel safe telling you the truth.
Ask direct questions. "Have you been using pills that weren't prescribed to you?" "Have you tried heroin or fentanyl?" Frame these conversations around concern for their safety rather than judgment of their choices.
Look for physical evidence carefully, but avoid violating trust unless you have serious safety concerns. Finding pills, syringes, burnt spoons, or other paraphernalia requires immediate action.
Connecting With Professional Help
The Canadian Centre for Addictions provides specialized treatment programs for young people struggling with opioid use. These programs recognize that teens need different approaches than adults. Age-appropriate therapy, family involvement, and educational support all play crucial roles.
Professional assessment determines the severity of use and the appropriate intervention level. Some teens benefit from outpatient counselling. Others require residential treatment to safely detox and address underlying issues. Medication-assisted treatment—using buprenorphine or methadone under medical supervision—often provides the best outcomes for opioid recovery.
Family involvement matters tremendously. Parents need education about addiction, recovery processes, and how to support their teen without enabling. Many programs include family therapy sessions that rebuild trust and communication.
Long-Term Recovery Support
Recovery isn't a straight line. Relapse happens frequently, especially in the first year. This doesn't mean failure—it means the person needs adjusted treatment approaches or additional support.
Aftercare planning begins before treatment ends. This includes identifying triggers, developing coping strategies, connecting with support groups, and establishing regular check-ins with counsellors. Schools may need to provide accommodations. Friends might need to change.
Treatment programs address not the substance use but the underlying issues that contributed to it. Mental health disorders require ongoing treatment. Academic stress needs management strategies. Family dynamics might need adjustment. Social skills development helps teens connect with peers in healthier ways.
The Reality Check Ottawa Needs
Seven years after Chloe Kotval's death, Ottawa's teen opioid epidemic has worsened in almost every measurable way. Deaths have increased. The drug supply has become more toxic. Treatment access has decreased. Mental health challenges have intensified.
Yet we've also learned valuable lessons. Harm reduction saves lives. Naloxone accessibility matters. Education about fentanyl risks works. Early intervention prevents progression to severe addiction.
The data confirms Ottawa faces an opioid crisis among young people. The real question is whether communities will commit the resources and political will needed to implement evidence-based solutions.
Every teen who experiments with pills faces potentially lethal risk from the fentanyl-contaminated drug supply. Parents who think their child is immune because they're a "good kid" from a "good family" in a "good neighbourhood" need to understand: this crisis doesn't discriminate.
The Canadian Centre for Addictions offers hope through comprehensive treatment programs designed specifically for young people. Recovery is possible. Lives can be saved. But it requires recognizing the problem, overcoming stigma, and accessing professional help.
FAQ
What is the opioid epidemic, and why is it dangerous for teens?
The opioid epidemic refers to the sharp increase in opioid-related deaths and overdoses across Canada since the mid-2010s, driven primarily by fentanyl contamination of the illicit drug supply. Teens face extreme danger because fentanyl is 50-100 times stronger than morphine, making even first-time experimental use potentially fatal.
How common are teen deaths from opioids in Canada?
Opioid-related deaths among Canadian teens and young adults (ages 15-24) tripled between 2014 and 2021, with emergency department visits quadrupling during the same period. Fentanyl is now involved in 94% of youth opioid deaths, and approximately half of these deaths occur among young people without diagnosed opioid use disorders.
What should parents or caregivers do if they suspect opioid use?
Act immediately but approach calmly with direct, non-judgmental questions about drug use while looking for physical signs like constricted pupils, drowsiness, and behavioural changes. Contact the Canadian Centre for Addictions or another professional for assessment—don't try to handle this alone.
What are the main warning signs of opioid addiction in teenagers?
Physical signs include constricted pupils, unusual drowsiness, slurred speech, coordination problems, weight changes, and flu-like symptoms that may be withdrawal. Behavioural red flags include stealing prescription medications, increased secrecy, new friend groups, declining school performance, extreme mood swings, and financial problems.
How does mental health relate to teen opioid use?
Mental health challenges and opioid use are deeply interconnected, with anxiety, depression, trauma, and suicidal ideation ranking among the most common reasons teens misuse prescription opioids. Many young people self-medicate mental health symptoms rather than accessing appropriate therapy. Effective treatment must address both issues simultaneously through integrated care.





